What is the purpose of World Sight Day?
Worldwide, the WHO (World Health Organization) and IAPB (International Agency for the Prevention of Blindness), launched the Vision 2020 program in 1999.
Observed every year on the second Thursday of October, World Sight Day was established as part of Vision 2020.
This program’s objective is to inform the general public and decision-makers about common eye issues so that each individual and different organizations can take action to prevent blindness.
WHAT IS BLINDNESS?
According to the NPCB (National Programme for Control of Blindness), total blindness is defined as a VA of 3/60 in the better eye with full refractive correction and/or a vision field less than 10 degrees from the fixation point.
Visual impairment is a VA of less than 6/18 in the better eye with full refractive correction.
In 1976, India began the 100% centrally sponsored National Programme for Control of Blindness (NPCB). The purpose of the project is to help prevent avoidable blindness.
Approximately 90% of blindness is either curable or avoidable.
This type of blindness is more common in people with low socioeconomic backgrounds, among illiterates, and old age, typically over 80, and it seems to affect women more than men.
The National Health Policy of India in 1983 reminded that blindness was a significant public health issue and set a goal to lower the prevalence rate of blindness from 1.4% to 0.3% by 2020.
By lowering the prevalence rate to 0.36, we have nearly but not quite achieved our goal. The updated target is to reduce the disease burden from current levels and the prevalence of blindness to 0.25 percent by 2025.
PREVALENCE OF BLINDNESS:
WHO mentions that at least 2.2 billion people worldwide suffer from near or distant vision impairment. It is estimated that nearly half of these cases, or 1 billion, involve vision impairments that could have been avoided or are still unresolved.
Uncorrected refractive errors and cataracts are the main causes of vision loss and blindness, followed by age-related macular degeneration, glaucoma, diabetic retinopathy, and corneal opacity.
Out of all blindness in India, 68.11% is treatable, 24.79% is preventable, implying that roughly 93% is avoidable, and only 7.10% is not preventable.
NPCB focuses on the following conditions to prevent blindness in India.
- Cataract: Major cause of preventable blindness in patients over 50-year-old age group
- Uncorrected refractive error
- Corneal blindness
- Glaucoma
- Diabetic retinopathy
CATARACT
Age-related or senile cataracts are the most common cause of cataracts. Patients over 50 years of age are more likely to experience this.
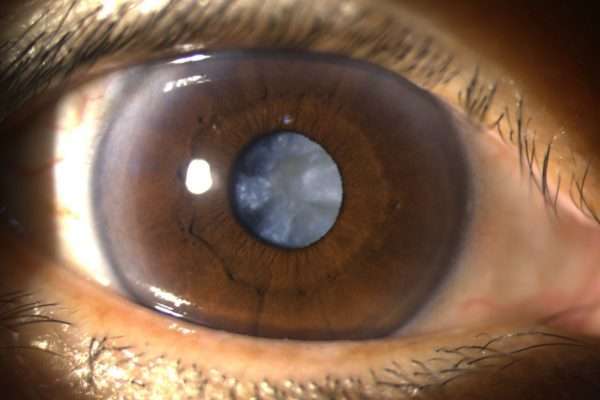
Other causes may affect younger populations as well. These are trauma, eye diseases such as high myopia, systemic illnesses such as diabetes, nutritional deficiency, radiation exposure, etc.
Symptoms
The majority of patients with cataracts in the early stages won’t even be aware that they have them until they go in for a routine eye exam. This is because cataracts gradually reduce vision both near and far, cause reduced night vision, and glare, making it challenging to drive at night.
TREATMENT:
Surgery is the only available treatment for cataract.
In cataract surgery, the surgeon exchanges the eye’s cataractous lens with an artificial intraocular lens, or IOL.
UNCORRECTED REFRACTIVE ERROR
Visual development and learning to see continue throughout early childhood. At this age, the child starts to focus and develops the binocular vision and depth perception.
The visual development will not be complete during this time if there is any obstruction in the visual processing, and the child may experience visual problems like amblyopia, squint, or strabismus.
Therefore, early vision screening and management are essential.
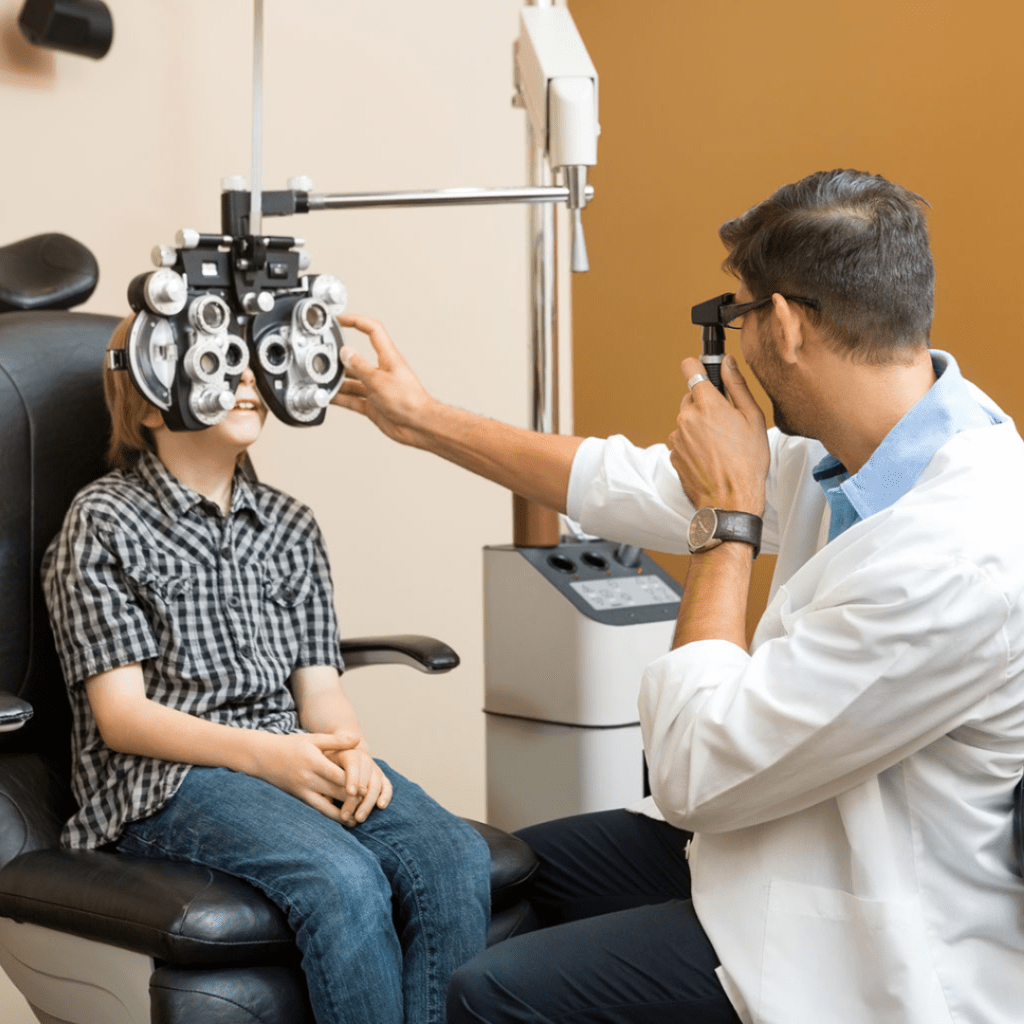
WHEN TO TAKE YOUR CHILD FOR EYE EXAMINATION?
Ideally, just before starting school, every child between the ages of 3 and 4 should have a routine eye exam.
If one or both parents have high power, it is best to take a baby to the eye doctor when they are a year old.
A preterm infant’s fundus needs to be checked for retinitis of prematurity within 30 days of birth.
CAUSE OF REFRACTIVE ERROR
Genetics play a major role in refractive error, which children inherit from their parents. However, a child may still experience refractive error even if both parents have normal vision or are emmetropes.
Research suggests that environmental factors, such as an increase in close work (reading, writing, using screens, etc.), can aggravate a person’s inherited tendency toward short or nearsightedness.
CORNEAL OPACITY/BLINDNESS
Understanding corneal blindness is crucial because, according to the WHO, it is one of the leading causes of blindness and vision loss in the world. Most importantly, this blindness is treatable.
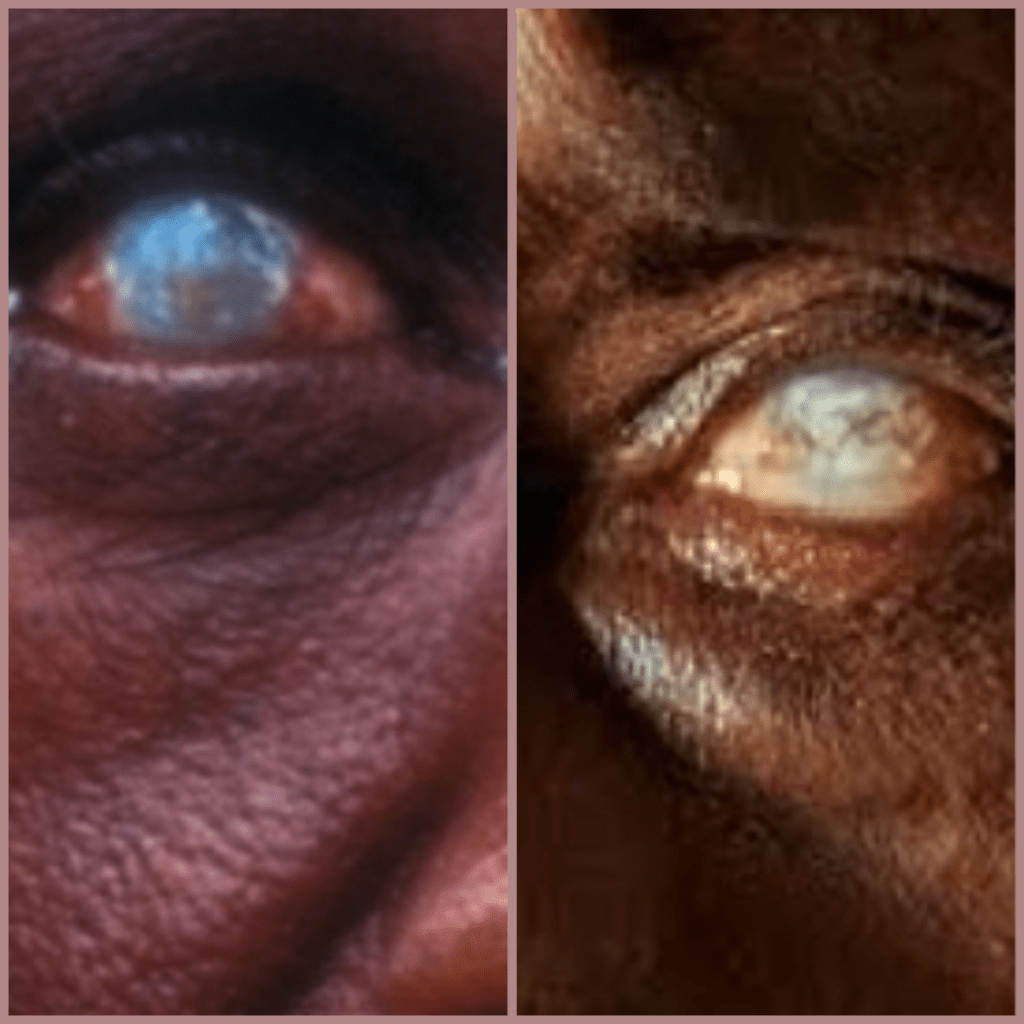
The causes include:
- Corneal dystrophy
- Corneal degeneration
- Corneal infection healed by scarring
- Trauma or chemical injury to the cornea
- Vitamin A deficiency in children can lead to corneal blindness
- Keratoconus- a condition in which the normal sphere-shaped cornea is conical
According to the National Programme of Control of Blindness (NPCB), 1–1.2 million Indians have corneal blindness in both eyes, and 5–6 million have it in just one. We need to collect about 2 lakh corneas each year to fulfill the approximate 1 lakh annual demand for corneal transplants.
Additionally, according to the NPCB, between 25 000 and 30 000 names are added to this list annually. There aren’t enough donor corneas available, despite the fact that we have hospitals, eye banks, and trained doctors for corneal transplants.
WHAT IS A CORNEAL TRANSPLANT?
The eye’s outer layer called the cornea is transparent like the glass in your watch. In the case of the scratched or opaque watch glass, you will be unable to read the time accurately, which is why you need to replace it. Similarly, in a corneal transplant, the diseased cornea is replaced with a healthy and clear donor cornea to see clearly.
Our society is heavily burdened by corneal blindness. In order to bridge the growing gap between the supply and demand for corneas, we must raise awareness about eye donation. We require a great deal of corneal transplants. Imagine not having sight while residing in this lovely world. After death, giving someone your sight is a lovely act of kindness.
PROCEDURE FOR DONATING EYES
If you want to donate your eyes but are unsure of how or where to do it, simply follow the steps below:
1. Go to your nearest eye back and complete the eye donation form.
2. You will be given a donor card.
3. Inform your family about your wish to donate.
4. Raise awareness. At least two people can receive sight from one person. Some specialised transplantation techniques split a single cornea into two parts, so one donor with two eyes can gift vision to four others.
When a family member who pledged their eyes passes away, this process must be followed.
- Contact the nearest eye bank.
- Remember that the corneas must be retrieved within 6 hours of death.
- Close the eyelids and cover them with a moist cloth or cotton and keep it moist till the medical team arrives.
- Till then, keep the head raised with a pillow.
- Keep the death certificate ready.
- Meanwhile, switch off the fan and AC, where the body of the deceased is kept.
GLAUCOMA
Glaucoma is a group of diseases causing progressive damage to the sight which finally leads to irreversible blindness. People with glaucoma may not even be aware that they have it until it is too late because in many cases it is painless and affects the peripheral vision first.

The remaining vision in people with glaucoma can be preserved by receiving early treatment and routine monitoring.
People need to be made aware of the significance of receiving an annual, comprehensive eye exam from a qualified eye doctor.
The visual field becomes restricted as a result of the initial peripheral vision loss. As the condition worsens, the peripheral vision gets increasingly limited, resulting in tunnel vision and eventually going completely blind.
TREATMENT
In most of cases, glaucoma can be stopped from progressing by using eye pressure-lowering eye drops and /or laser therapy.
Once the eye drops are prescribed by your ophthalmologist, these have to be used regularly and diligently. Make sure you are going for your regular follow-ups.
In some cases, surgery is important especially when
1. IOP is not coming down even after maximum medical therapy.
2. The patient is not compliant with the medication or follow up/ or it’s not possible to follow up regularly.
3. Intolerable side effects with topical medications.
4. The patient opts for surgery instead of lifelong medication.
The surgical options include trabeculectomy, minimally invasive glaucoma surgery or MIGS, glaucoma implants or valves etc.
DIABTEIC RETINOAPTHY
Blood is delivered to the retina by the retinal arteries. These arteries’ walls deteriorate as a result of elevated blood glucose levels. The vessels start to leak as a result, resulting in swelling (hard exudates, edoema) and haemorrhages within the layers of the retina. Diabetic retinopathy is the medical term for this.
The two main types of DR are non-proliferative and proliferative.
- Non Proliferative diabetic retinopathy (NPDR):
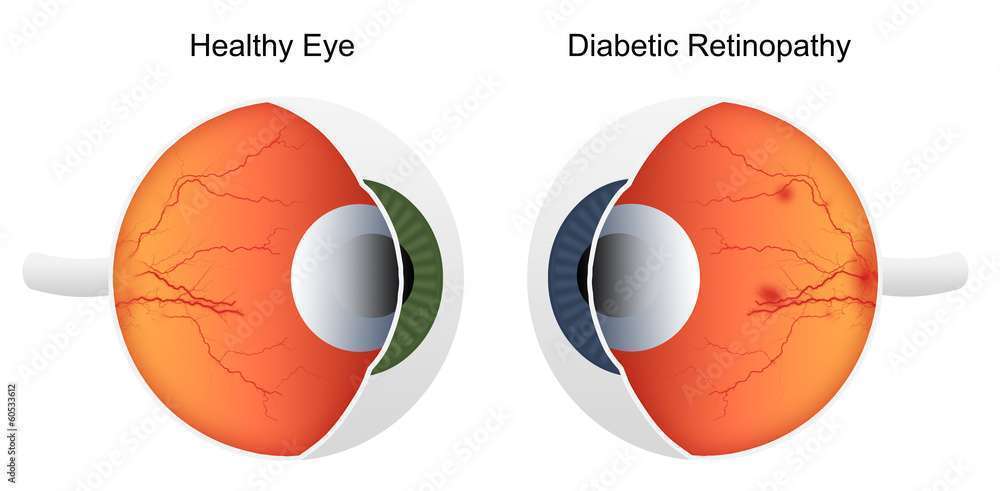
Diabetes weakens the retinal vessel wall, which results in microaneurysms, a condition where the vessel lumen protrudes outward. Red dots are the hallmark of retinal microaneurysms.
Retinal haemorrhage occurs within the layers of the retina when these microaneurysms burst. Hard exudates are yellow deposits that are caused when proteins and lipids leak from the porous retinal wall.
- Proliferative Diabetic retinopathy (PDR):
The retina in this stage is under a great deal of stress, which results in a lack of oxygen, which leads to the release of VEGF (Vascular Endothelial Growth Factor), which has the function of growing new blood vessels.
However, because these new vessels are fragile and prone to bleeding, they can cause even graver conditions like bleeding in the retina or vitreous. The retina’s new blood vessels may also pull on it, leading to retinal detachment.
TREATMENT:
A healthy diet and prescription medications (oral hypoglycemic/insulin) may be sufficient for treating diabetic retinopathy in cases of mild-moderate non-proliferative diabetic retinopathy. It is necessary to follow up frequently.
Proliferative diabetic retinopathy (PDR), one of the most severe forms of diabetic retinopathy, calls for laser surgery and/or anti-VEGF injections in addition to proper blood sugar management.
Diabetic Macular edema (DME)
The retinal vessels near the macula, the core of the retina and the source of sharp central vision, become leaky as a result of the disease called DME. This causes a serious loss of vision.
Lasers are used to seal the leaky vessel directly for focal leaks, but anti-VEGFs are a better option for diffuse leaks.
COMPLICATIONS OF DIABETIC RETINOPATHY
If diabetic retinopathy worsens, this can progress to the advanced stage. The complications include:
- Vitreous hemorrhage: The new fragile vessels can bleed into the jelly inside the eye, which is called a vitreous hemorrhage. One may notice many floaters in front of the eyes if the condition is mild or in severe cases, there can be loss of vision.
- Retinal detachment: The new vessels or scar tissue can even pull the retina and cause retinal detachment.
- Glaucoma: The VEGF can cause growth of new blood vessels in the front part of your eye (iris) which may interfere with the drainage of the fluid out of the eye, causing increased pressure within the eye. This raised pressure can damage the nerve of the eye which is involved in image transmission to the brain. The condition is known as glaucoma
- Irreversible blindness: A complicated case of diabetic retinopathy along with diabetic macular edema/vitreous hemorrhage/retinal detachment/glaucoma or a combination of these conditions can lead to irreversible blindness.
How the NPCB is responding
The program’s best practices are as follows:
- The program provides for the establishment of Multipurpose District Mobile Ophthalmic Units in District Hospitals of States/UTs to provide eye care services to every nook and cranny across the country.
- As a new initiative under the program, there is a provision for giving away free glasses to elderly people with presbyopia so they can perform close-up work. It is necessary to speed up the process in all states.
- The focus is on providing comprehensive eye care, including treatment of conditions other than cataracts, such as glaucoma, diabetic retinopathy, and retinopathy of prematurity (ROP). To completely eradicate preventable blindness from the nation, these emerging diseases require urgent attention.
- Ensuring the establishment of superspecialty clinics for all significant eye diseases, such as diabetic retinopathy, glaucoma, retinopathy of prematurity, etc., in state level hospitals and medical colleges across the nation.
- With tele-ophthalmology facilities at PHC/Vision Centers, eye diseases can be diagnosed and treated more effectively, especially in hilly areas.
- Creation of a network of eye banks and donation centers connected to medical schools and RIOs to encourage the timely and transparent collection of donated eyes.
HOW TO PROTECT YOUR EYES?
1. Annual routine health checkups:
The eyes can suffer from high blood pressure, high cholesterol, and high blood sugar. Numerous autoimmune disorders and infections can also cause irreparable harm that impairs vision and even causes blindness. Keeping an eye on your overall health is crucial.
2. Routine eye check up:
Maintaining the health of the eyes requires routine eye examinations by a qualified eye specialist. Regular check-ups can identify diabetic retinopathy, glaucoma, and cataracts at an early stage, which simplifies management.
3. Sunglasses with UV protection:
UV rays can harm the macula or cause macular degeneration, a condition that impairs a patient’s central vision. In addition to this, harmful UV rays are also known to cause, cataracts, pterygium (a fleshy growth on the white part of the eyes), skin cancer around the eyes, wrinkles, etc.
4. 20-20-20 rule
Use the 20-20-20 rule to prevent eye fatigue when using digital screens for extended periods of time. After every 20 minutes of computer work, look at an object 20 feet away for 20 seconds.
5. Strict blood sugar control:
Uncontrolled high blood sugar causes crippling eye conditions diabetic retinopathy and diabetic macular edema, which can result in blindness. Maintaining healthy blood sugar levels is criticalby following a healthy diet and taking medication as prescribed by a doctor.
6. Eat a balanced diet.
Food that is high in healthy fats and antioxidants can help to promote eye health.
7. Contact lens maintenance:
It is advised that people who wear contacts handle them after washing their hands with soap and water, take them off with clean hands before going to bed, and clean them with contact lens solution.
8. Quit smoking:
One of the main risk factors for many eye diseases is smoking. For example, dry eyes, under-eye dark circles, optic neuropathy, inflammation within the eyes, cataracts, AMD (Age-related Macular Degeneration), glaucoma, diabetic retinopathy, etc.
As a result, healthy behaviours like quitting smoking can help shield the eyes from a number of diseases that can be avoided. Find out why smoking is bad for your eyes here.
9. Reduced screen time:
The American Academy of Pediatrics recommends that children younger than 18 to 24 months should not use digital media (other than video chatting).
The AAP suggests limiting screen time for children between the ages of 18 months and 5 years to no more than one hour per day(spread throughout the day) and emphasizing educational content.
