WHAT IS OSA OR OBSTRUCTIVE SLEEP APNEA?
Obstructive sleep apnea is defined as airflow obstruction (>90% collapse of the airway in the throat) for >10 seconds in the presence of breathing effort. In other words, a person who is sleeping stops breathing for a moment. Sleep apnea patients may stop breathing as many as 100 times an hour, or even more, for up to a minute each time.
OSA is a very common problem affecting 2-9 % of general population
PATHOPHYSIOLOGY
In REM sleep or rapid eye movement sleep, our muscles have the lowest tone. Normally, the tongue falls back when lying supine, but not so far as to obstruct the airway.
A person with OSA may have an increase in fat at the back of the throat. When the tongue muscle tone drops during REM sleep, it falls on this thickened back surface of the throat, causing the person to snore due to narrow airway.
An obstruction of this airway by more than 90% results in cessation of breathing or apnea.
This results in the oxygen saturation dropping. A decrease in oxygenation in the body signals the brain that something is wrong.
When the brain awakens, the tongue muscles are tense, releasing the obstruction and allowing snoring to resume.
Therefore OSA is a cycle of loud snoring followed by silence (apnea) followed by a snort and then snoring. In most cases, the person sharing the bed can help diagnose OSA.
RISK FACTORS:
- Male: OSA is more common in males due to more fat in the neck. Women are at same risk after menopause.
- Obesity: Risk increases by 10-14 times
- Age: >50 years age group
- Race: Increased incidence in Asian
- Genetic: Risk increases with positive family history of OSA in 1st degree relative
- Genetic disorder such as Down’s Syndrome
- Anatomy: Large tonsils, Retrognathias, neck circumference >43 cm
- Nasal obstruction: Allergic rhinitis
- Lifestyle related: Alcohol consumption just before sleep time, tobacco consumption
SIGNS AND SYMPTOMS
- Apnea: During REM sleep when the muscle tone is lowest, there are several episodes each night that the patient will experience cessation of breathing due to >90% collapse of airway in the throat for 10 seconds.
- Snoring: Continuous, loud, and bothersome snoring interrupted or stopped by apneas, followed by snorting and repeated several times during the sleep cycle.
- Multiple micro awakenings
- Insomnia
- Nocturia
- Headache in the morning
- Confusion
- Dry or sore throat
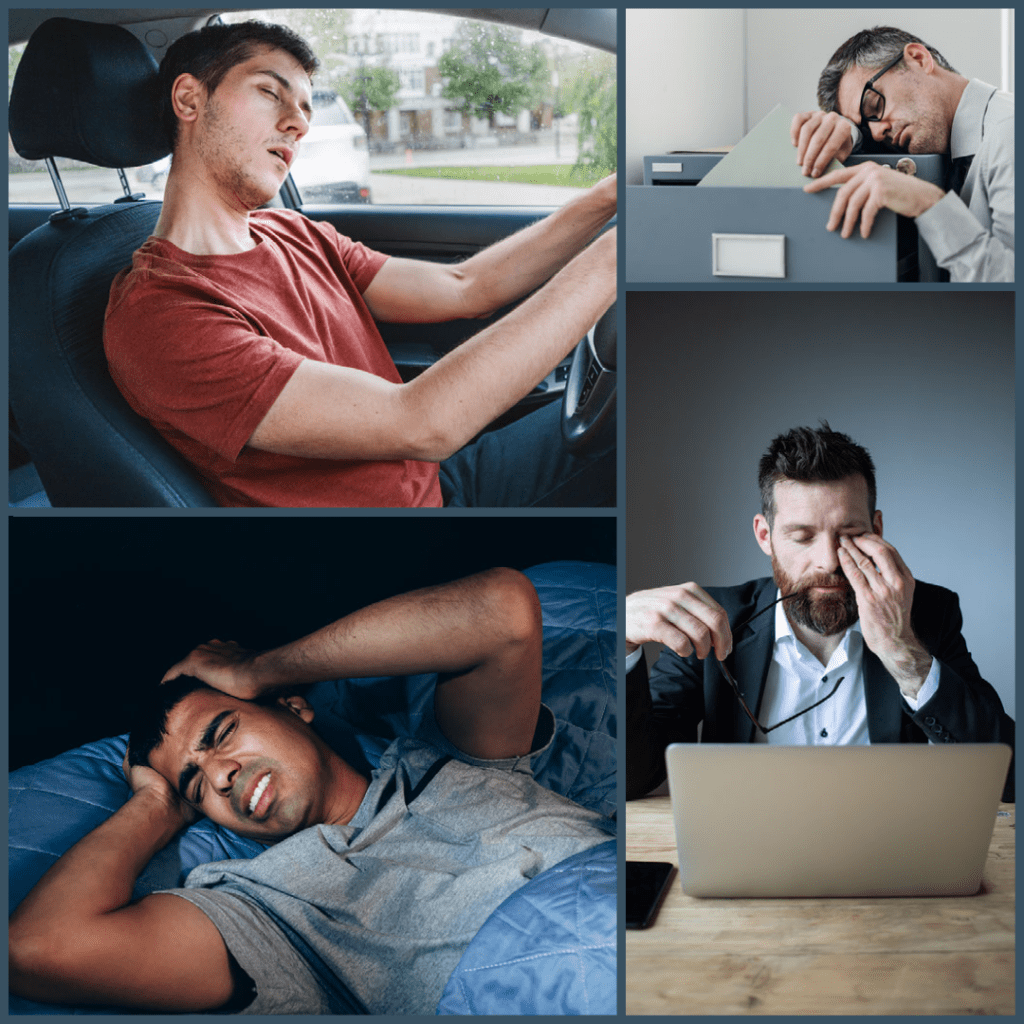
- Excessive daytime sleepiness
- Fatigue
- Decreased concentration and memory
People with obstructive sleep apnea are more likely to suffer a heart attack, arrhythmia, stroke, diabetes, hypertension, mental slowdown, depression, and memory loss. The risk of motor vehicle accidents increases if they are driving while drowsy.

OSA has a great impact not only on overall health, but also on eye health.
IMPLICATIONS OF OSA ON EYES:
Ocular manifestations of OSA derive from mechanical and vascular effects of the syndrome. These include Floppy Eyelid Syndrome (FES), Nonarteritic Anterior Ischemic Optic Neuropathy (NAION), Central Serous Retinopathy(CSR), Retinal Vein Occlusion(RVO), and glaucoma.
1. FLOPPY EYELID SYNDROME
In FES the upper eyelids evert easily when traction is applied upward.
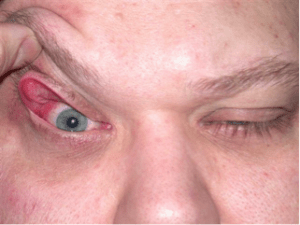
An apneic event can produce transient ischemia in lid tissue, exacerbated by hypoxia. As normal breathing resumes, reperfusion oxidation injury may cause continuous inflammation of the lids.
Consequently, the eye may experience foreign body sensation, dryness, redness, or swelling of the eyelids as a result of exposure.
In patients with dry eyes, excessive tearing may be a reaction to underlying dryness. A referral to an ophthalmologist may assist in evaluating corneal pathology in patients experiencing these symptoms.
Thus OSA patients’ FES is attributed both to chronic inflammation and to underlying connective tissue weakness
2. NONARTERITIC ANTERIOR ISCHEMIC OPTIC NEUROPATHY
NAION is characterized by a sudden, painless, unilateral, irreversible, and nonprogressive loss of vision that often occurs without any warning.
Patients with untreated OSA are 16% more likely to develop NAION than those without OSA. The contralateral eye of patients with NAION is at a 15% risk over a five-year period.
There is usually a sudden loss of vision upon awakening, suggesting nocturnal hypotension as a contributing factor. Thus, patients taking multiple hypertension medications are at higher risk of developing this condition.
In addition, intracranial pressure increases during apneic episodes. A high intracranial pressure results in inadequate perfusion of the optic nerve, which may cause NAION.
3. CENTRAL SEROUS RETINOPATHY (CSR)
CSR is an idiopathic retinal detachment caused by serous fluid collecting underneath the retina.
Patients with OSA have higher levels of circulating epinephrine and norepinephrine thus leading to increased sympathetic stimulation. This causes endothelial dysfunction to occur on the blood-retinal barrier, which leads to accumulation of subretinal serous fluid and retinal detachment.
4. RETINAL VEIN OCCLUSION

RVO is of three types, Branch Retinal Vein Occlusion, Central Retinal Vein Occlusion, and Hemi retina vein occlusion.
The more common of these occlusion events is occlusion of the branch retinal vein system, while occlusion of the central retinal vein system is less common.
After diabetic retinopathy, retinal vein occlusion (RVO) is the second most common cause of blindness from vascular disease.
OSA affects blood autoregulation, causes slowing of blood flow, and changes in the microvasculature. There is often an association between RVO and blood stagnation and hypercoagulability.
In some cases, hypoxemia and elevated nocturnal intracranial pressure may cause venous occlusion in OSA. A hemodynamic change in the central retinal artery can cause compression of the adjacent retinal vein thus contributing to the implication of OSA in RVO.
5. GLAUCOMA
Among the leading causes of blindness worldwide, glaucoma ranks second. Glaucoma is characterized by chronic, progressive optic neuropathy that results in significant visual field defects and characteristic cupping of the optic nerve seen on fundoscopic examination.
The exact cause of OSA leading to glaucoma is unknown, but it appears to be caused by hypoxia or decreased oxygen in retinal vessels during apneic episodes. This affects the health of the optic nerve that is perfused by these retinal vessels.
Oxidative stress, poor perfusion, inflammation, and conditions associated with poor blood supply to the optic nerve head, such as obesity, hypertension, and diabetes, are also possible confounding factors.
Some studies suggest that treating OSA may have an effect on glaucoma progression.
TREATMENT
1. Lifestyle modification:
- Weight loss
- Restricted alcohol and tobacco consumption. It is recommended to avoid drinking alcohol for at least 4-6 hours before sleep.
- Sleep on one side instead of sleeping on the back.
2. Nasal CPAP (Continuous Positive Air Pressure) machine: A plastic hose connects the machine to the mask the patient wears. While he/she sleeps, the machine pushes pressurized air into their airways to prevent them from closing.

3. Tonsillectomy surgery to remove tonsils in case of enlarged tonsils and/or adenoids
As a result of OSA, patients may suffer from a wide variety of ailments, some of which can be fatal. Timely diagnosis and treatment is the key. It is best to see a doctor in case of any vision problems.

