WHAT IS COVID-19?
Coronavirus (COVID-19) is a disease caused by the Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus). An RNA beta coronavirus with unique encapsulation and high contagiousness was first discovered in Wuhan, China, in early December 2019. Since then, it has rapidly spread throughout the world.
TRANSMISSION OF THE VIRUS
COVID 19 virus spreads just like flu or common cold. This includes:
1. Infected respiratory droplets: When an infected person coughs or sneezes, infectious droplets are released into the air and can be breathed in by others nearby.

2. Fomites: By directly handling the COVID19 viruses or by touching things or materials that have had infectious droplets fall on them, our hands can become contaminated. The infection can spread from the contaminated hands to the mucous membrane of the mouth, nose, or eyes through touching.
People ought to often wash their hands and cover their mouth and nose when coughing to stop the spread of germs.
HOW DOES COVID-19 REACH THE EYES?
Infected people can carry COVID-19 virus in their tears. How it reached the ocular secretions is still unclear. But there have been several hypotheses related to this:
- Migration from the nasopharynx,
- Spread through bloodstream carrying infection from the upper respiratory tract to the nasolacrimal duct or lacrimal gland,
- Direct contact of eye tissues by infected respiratory droplets or aerosolized virus particles.
- Touching or rubbing of eyes with contaminated hands.
COVID EYE
The most typical signs and symptoms of COVID-19 are a persistent cough and a high body temperature. Even though the prevalence of ocular symptoms among COVID-19 individuals is lower and varies from 2-32%, there is now evidence that suggests eye issues may be either the first symptom of coronavirus infection or the sole symptom.
SYMPTOMS OF COVID EYE INFECTION:
The presentation, seriousness, and timing of ophthalmic symptoms vary. According to Wu et al., patients with severe systemic disease who have abnormal blood and inflammatory parameters are more likely to experience ocular signs.
Some of the commonly reported eye conditions are:
1. Conjunctivitis

Watery discharge, conjunctival redness, ocular discomfort, swollen eyelids, chemosis, and a feeling of a foreign body are some of the symptoms. The right handling and disinfection of anything that comes into contact with contaminated hands that touched the patient’s eyes are also important components of management. It is important to properly advise the patient not to rub their eyes. It’s crucial to use lubricating drops for comfort and topical antibiotic medicines to avoid secondary infections.
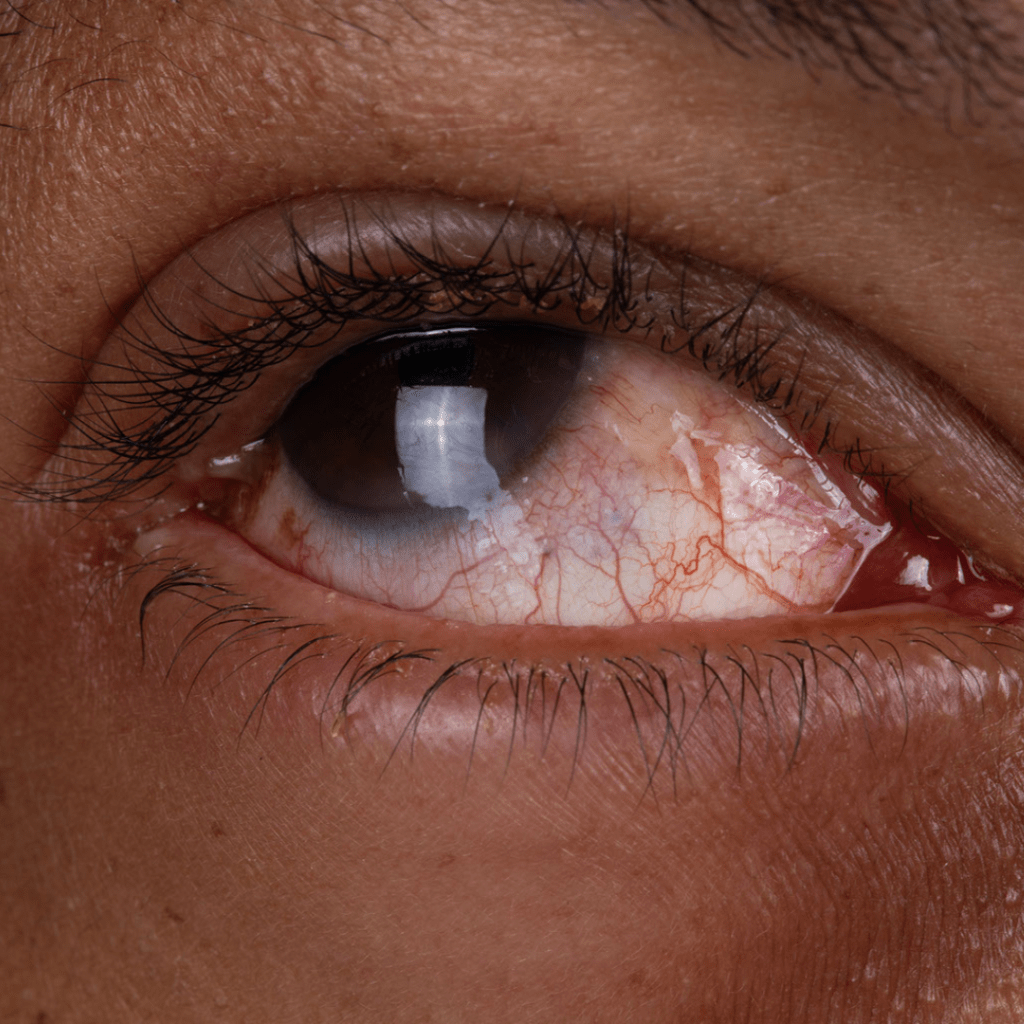
2. Episcleritis or inflammation of episcleral tissue.
This tissue is located above the white sclera and under the clear conjunctiva. It’s important to treat this with non-steroidal anti-inflammatory drugs and lubricating drops because it may result in pain and discomfort.
3. Acute anterior uveitis.
An inflamed iris and/or ciliary body, a muscle surrounding the iris, causes anterior uveitis. Pain, photophobia, floaters, and redness are some of the symptoms. Medications such as steroid eyedrops are used alongside rigorous monitoring by a physician.
4. RetinA:
The retina is the photosensitive layer in the back of the eye. Cases of cotton wool spot-like lesions and hemorrhages associated with COVID-19 infection have been observed. There are a number of causes of swelling, hypoxia, and occlusion in retinal vessels, including vascular, inflammatory, and neurological conditions. Symptoms include floaters, blurred vision or loss of vision, difficulty seeing in the dark etc.
5. Optic nerve inflammation or optic neuritis:
The nerve that carries visual information from the back of the eye to the brain is known as the optic nerve. This nerve’s inflammation can lead to pain, brief vision loss, and colour vision abnormalities. The use of steroidal therapy must be strictly regulated by a physician.
6. Restricted movement of the eye:
The literature has reported cases of cranial nerve III, IV, and VI palsies linked to COVID-19 within a few days of the onset of fever and cough, the majority lacking notable radiological findings. These cranial nerves control eye movement, thus when they become weak during or after a covid infection, it might result in painful and limited eye movement.
7. Rhino-orbital Mucormycosis:
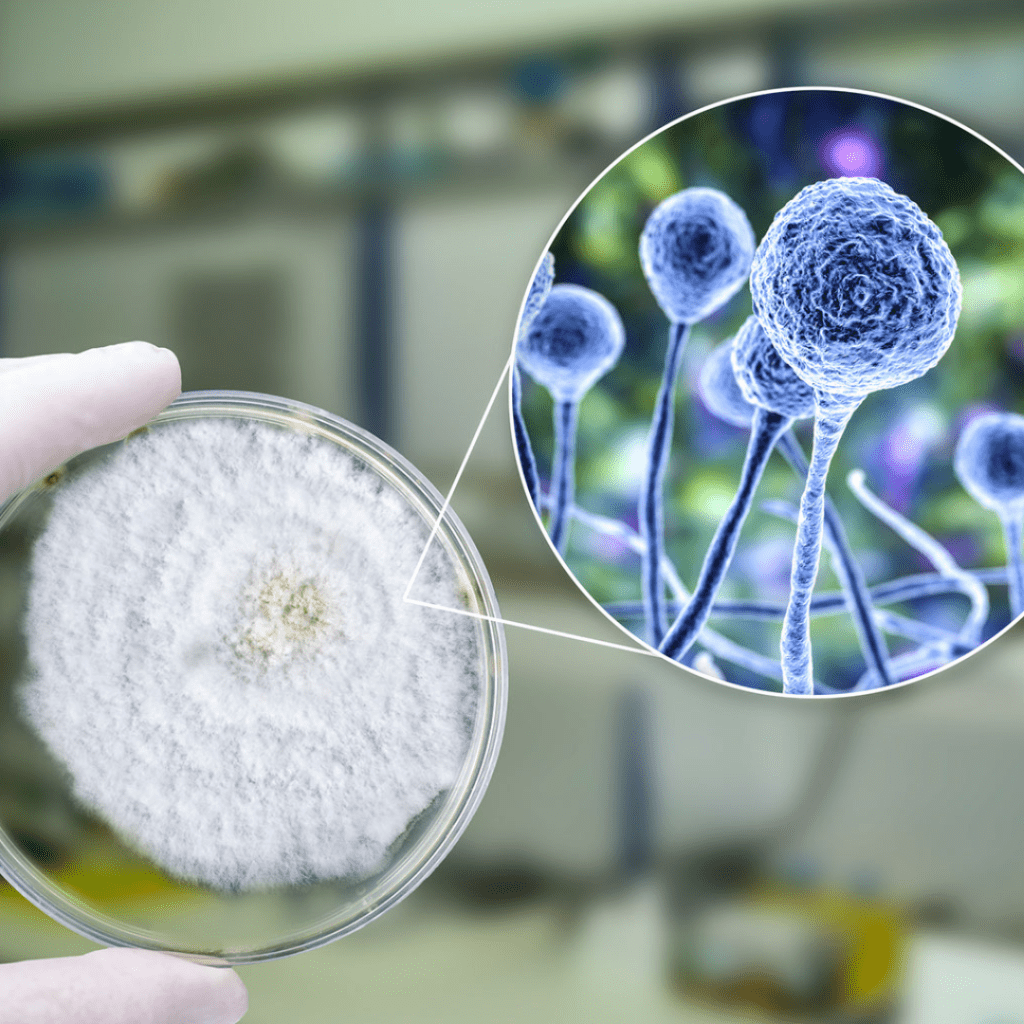
Patients with moderate to severe COVID-19 have reduced immune systems, making them more susceptible to the potentially lethal opportunistic infection known as mucormycosis. Furthermore, the widespread adoption of steroids, monoclonal antibodies, and broad-spectrum antibiotics in the fight against COVID-19 may cause the emergence or aggravation of preexisting fungi illnesses. Almost 70% of rhino-orbital-cerebral mucormycosis is seen in patients with uncontrolled diabetes and most of them have ketoacidosis at the time of presentation
A patient may present to an ophthalmologist with unilateral face or orbital pain, a headache, swelling around the eyes, double vision, or vision loss. A routine evaluation of a COVID-19 patient hospitalized with moderate to severe illness should include clinical eye tests such visual acuity charting, pupillary examination for light reflexes, and extraocular movements assessment.
The management includes using antifungal medications, vigorous surgical debridement, functional endoscopic sinus surgery or FESS. In a life-threatening situation, orbital exenteration within 4-72 hours might be the sole option. Even with treatment, there is a 50% mortality rate.
PREVENTION OF COVID EYE INFECTION

- Practice hand hygiene
- Do not touch or rub eyes
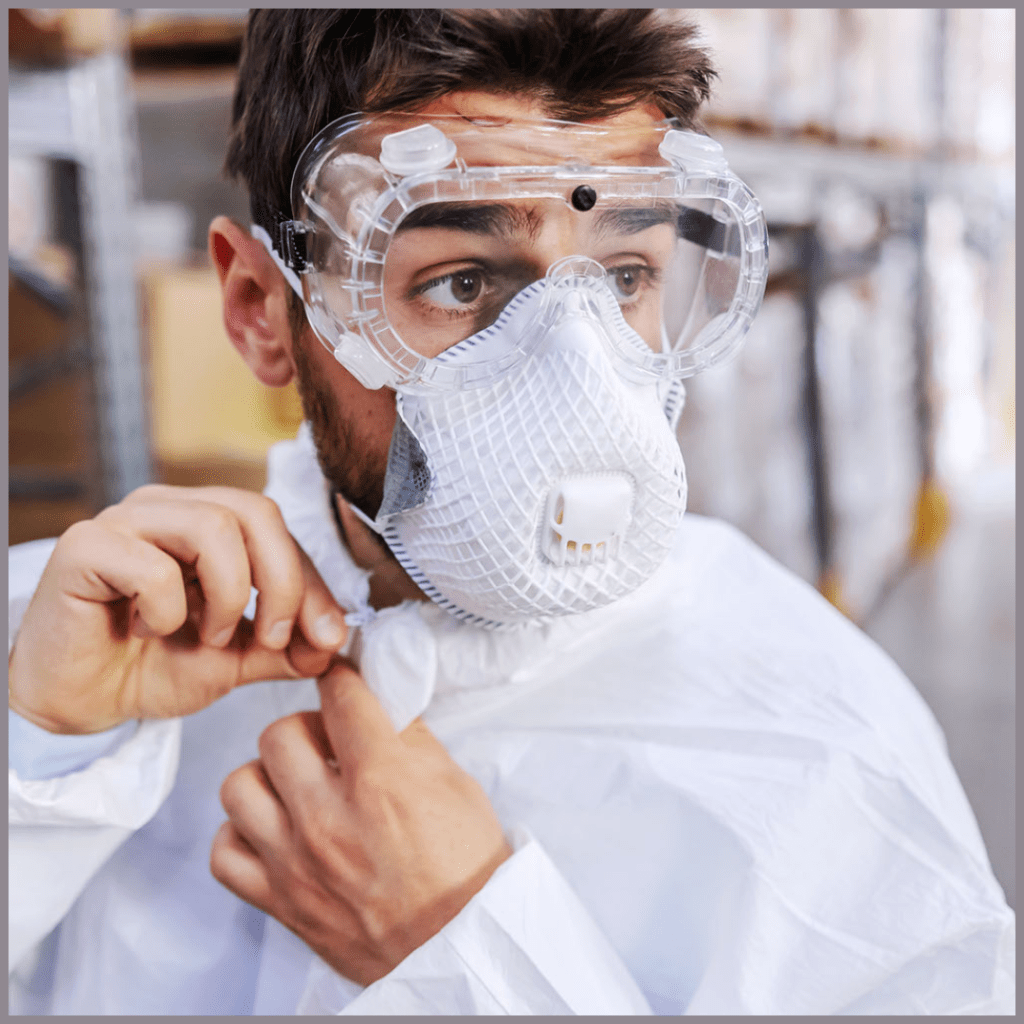
- When caring for patients with COVID, wear protective glasses
- Maintain safe distance
- Vaccinate
QUICK SUMMARY:
Throughout the Coronavirus outbreak, the signs, symptoms, occurrence, timing, severity, and response to therapy of COVID 19-infected patients have varied significantly. The patient should be aware of this and contact their eye doctor right away if they suffer redness, pain, blurring, or restricted eye movement when they are COVID positive or recovering from COVID. There are situations where the ocular manifestation was the sole sign of the COVID 19 virus. One of the most crucial aspects of recovering from COVID in individuals with uncontrolled diabetes is maintaining strict glycemic control.
