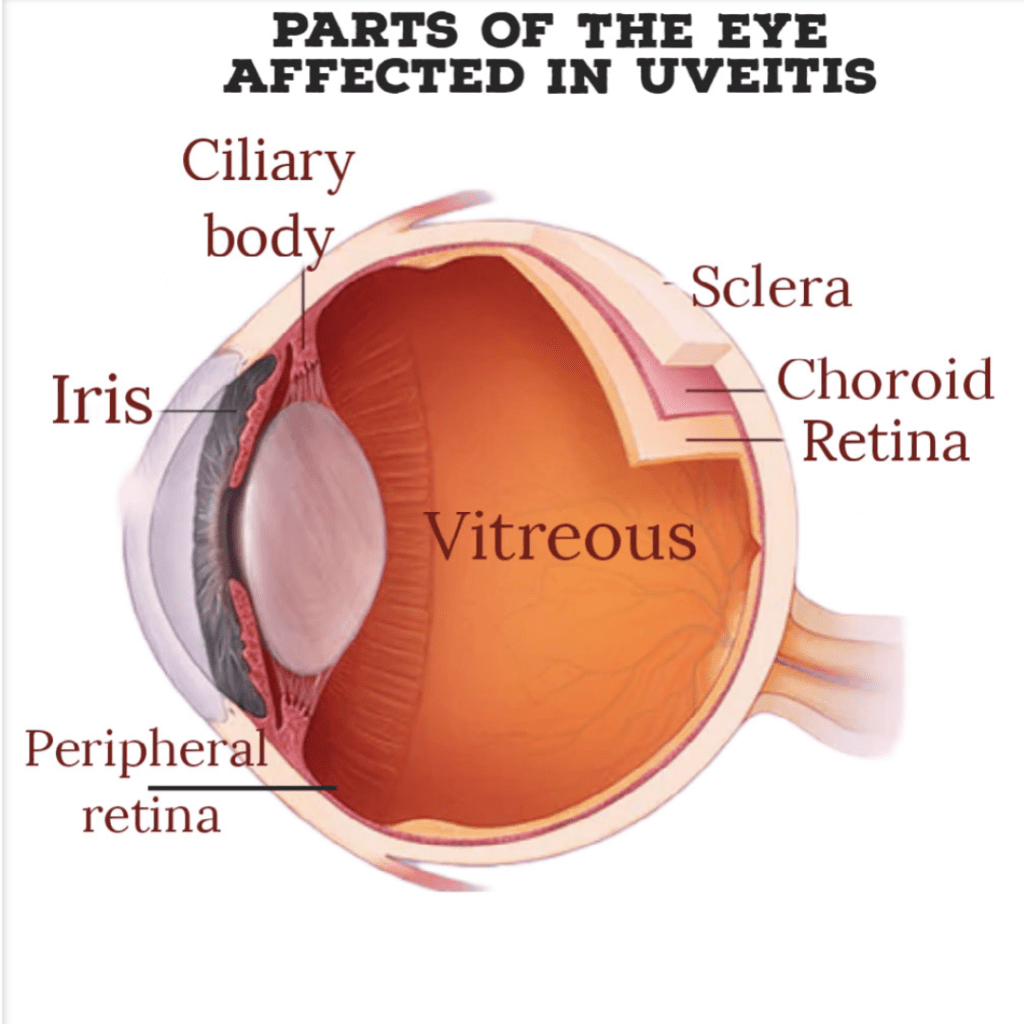
Uveitis refers to ocular inflammation or swelling inside the eye. It typically impacts the uvea, middle layer of the eye, but it can also affect other crucial eye structures which could result in permanent vision loss.
The uveal layer is present between the retina (light-sensitive layer at the back of the eye) and the sclera (white part of the eye).
It is divided into the following:
- Iris: the coloured part of the eye
- Ciliary body: muscle behind the iris which aids in the lens’s ability to focus.
- Choroid: layer of blood vessels present between the retina and the sclera.
Other structures affected by uveitis are:
- Retina, the light-sensitive innermost layer of the eye, and
- The vitreous: gel-like structure which fills the back of the eye.
What are the types of uveitis?
Uveitis can be classified into different types based on the affected structures:
- Anterior uveitis: Anterior uveitis, or iritis, affects the iris and ciliary body located inside the front part of the eye. Typically, it’s less severe and more common. The symptoms can appear suddenly and last for several weeks. Some types of anterior uveitis are persistent, while others fade but recur.
- Intermediate uveitis: Intermediate uveitis affects the peripheral retina and the vitreous. The duration of the symptoms can range from a few weeks to many years. This form can experience cycles of improvement and deterioration.
- Posterior uveitis: The posterior uveitis affects the retina and/or choroid at the back of the eye. The onset and duration of symptoms can vary and last for many years.
- Panuveitis: Panuveitis affects the entire uvea, from the front to the back of the eye. This condition is very serious.
SYMPTOMS:
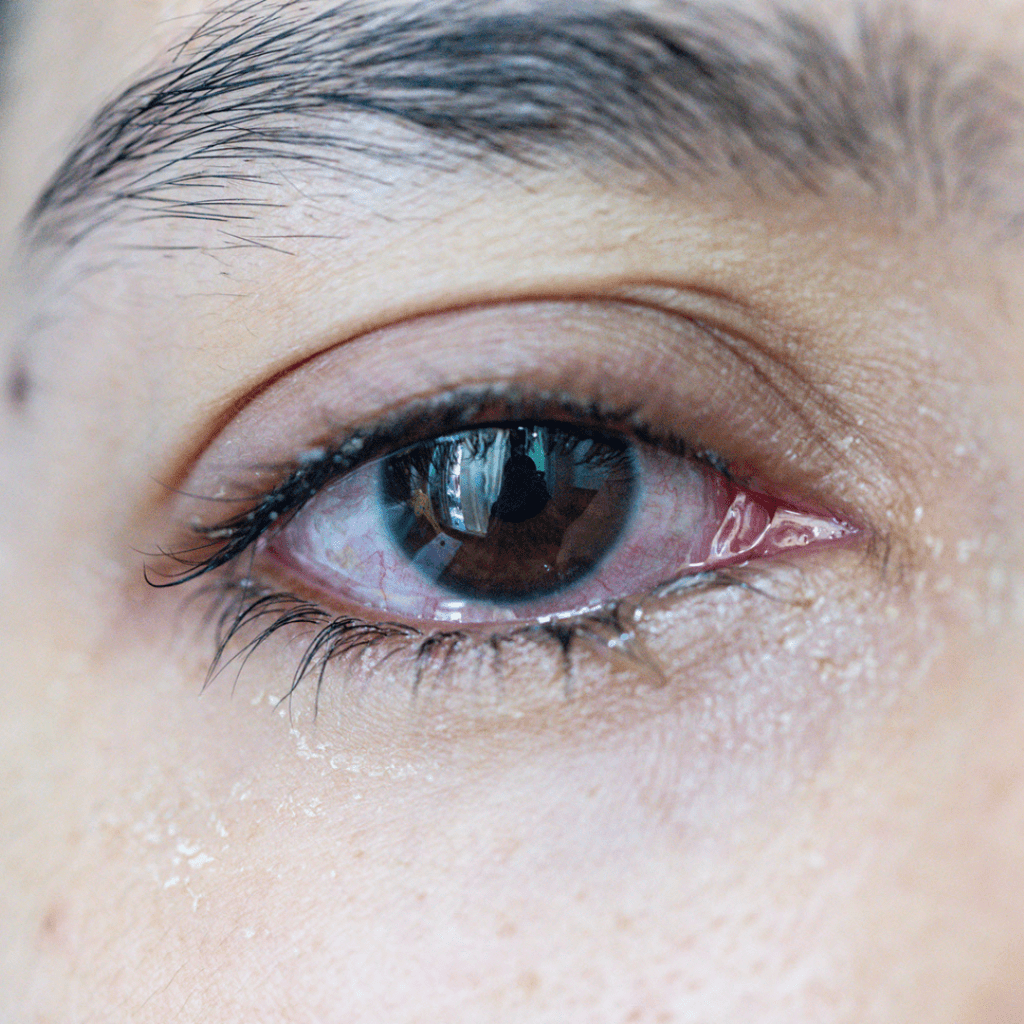
The warning signs of uveitis frequently appear suddenly and progressively worsen. They consist of
- Pain
- Redness
- Watering
- Photophobia
- Blurred vision
- Floaters
What causes uveitis?
Uveitis can affect either one or both eyes in people of all ages, including children. Uveitis may be caused by an infection, an injury, or an autoimmune or inflammatory condition. In many cases, there is no apparent cause.
- Idiopathic: cause not known
- Infections: Examples include toxoplasmosis, herpes simplex, syphilis, Lyme disease, tuberculosis, and cytomegalovirus (CMV) retinitis, among others.
- Autoimmune diseases: AIDS, rheumatoid arthritis, multiple sclerosis, and lupus are examples of autoimmune diseases;
- Eye injury
- Ocular cancer
- Smoking (cigars, cigarettes, or pipes) also increases risk of uveitis.
Diagnosis
Eye doctors are able to diagnose uveitis clinically. In some cases, however, diagnostic tests may be necessary to exclude infections or systemic diseases leading to uveitis.
They could consist of a physical examination, blood or skin tests, an eye fluid analysis, and imaging tests like X-rays.
Treatment
Uveitis can cause permanent vision loss and be very serious. To avoid complications and maintain vision, early diagnosis and treatment are crucial
1. Steroids:
- Eyedrops:
Ophthalmologists commonly use corticosteroid eye dops to treat uveitis. Following the schedule and tapering gradually according to the doctor’s advice is crucial.
- Injectables:
To control the inflammation, steroid injections into and near the eye may be necessary in certain circumstances.
- Systemic:
If topical or local steroid therapy fails to control uveitis, if there is bilateral or systemic involvement, or when the response is inadequate, systemic steroid therapy may be necessary.
- Implants:
Ozurdex (dexamethasone steroid implant; Allergan, Inc.) received FDA approval in September 2010 to be used in the management of uveitis. Through a 23-gauge needle, the Ozurdex device is implanted inside the eye. Dexamethasone reduces swelling for 4-6 months.
Steroids can have negative side effects and raise the risk of glaucoma and cataracts. It’s crucial to get routine eye exams if patients take steroids for uveitis to look for indications of these issues.
2. Mydriatic eyedrops:
These drops widen the pupil and relax the ciliary muscle, which eases pain. Ciliary muscle relaxation may cause blurred vision as the lens does not focus properly.
3. IMMUNOMODULATORY THERAPY:
Minimizing the use of corticosteroids and all of their numerous systemic and ocular side effects is one of the main objectives in the treatment of uveitis.
Immunomodulators, enable a doctor to lower the steroid dosage if it is causing significant negative health effects on the patient.
4. PARS PLANA Vitrectomy surgery:
The goal of therapeutic vitrectomy is to enhance vision by treating persistent uveitis, clearing the visual axis, and reducing inflammation in active disease. This procedure is more widely used in the treatment of intermediate uveitis and CME.
5. Management of infections and Autoimmune diseases:
The ophthalmologist collaborates closely with the other specialist to provide the patient with the best care possible when a systemic disease causing uveitis is present.
COMPLICATIONS ASSOCIATED WITH UVEITIS
1. Cataract:
One of the most frequent side effects in people with chronic uveitis is cataracts. Patients with uveitis are most likely to form cataracts if their inflammation is uncontrolled, persistent, and/or prolonged. Other risk factors include long-term topical, periocular, and/or systemic corticosteroids treatment.
2. Glaucoma:
About 20% of patients with uveitis develop glaucoma, a common complication of the disease. Inflammatory reactions can impair aqueous humor flow and lead to increased IOP. A steady increase in IOP can cause glaucomatous optic neuropathy and vision loss.
3. Uveitic macular edema:
This is a side effect of either acute or chronic uveitis. There is swelling in the macula and vision loss due to a buildup of fluid in the retinal layers. It is the primary cause of visual impairment in cases of uveitis.
4. Formation of new blood vessels in the eye (neovascularization):
A rare but serious complication of uveitis is neovascularization of the eye. Inside the eye, these new vessels are fragile and readily bleed. The retina and optic disc are the most common sites for formation of new blood vessels, although they can also develop in the iris, ciliary body, and choroid.
