What is Thyroid Eye Disease or TED?
TED results from inflammation (swelling) and damage to the tissues around the eye, including the muscles, fatty tissue, and connective tissue. About 90% of cases of TED are hyperthyroid, and 10% of patients either have a thyroid that is functioning normally (euthyroid) or that is underperforming (hypothyroidism, such as Hashimoto’s thyroiditis).
Graves disease and TED frequently coexist. Thyroid eye disease is present in between 25 and 50 percent of cases of Grave disease (GD). Graves’ disease (GD) is an autoimmune condition affecting the thyroid gland characterized by circulating autoantibodies that bind to the thyroid hormone receptor (TSHR) and cause hyperthyroidism and goiter.
RISK FACTORS:
- Smoking: Smoking directly impacts the possibility of developing TED, and continuing to smoke increases the likelihood that eye abnormalities will progress and become more severe. Additionally, smoking reduces the efficacy of thyroid eye disease treatments
- Thyroid function: At the time of diagnosis, 90% of TED cases have severe or uncontrolled hyperthyroidism, 6% have euthyroidism, 3% have Hashimoto thyroiditis, and 1% have hypothyroidism. Every six to twelve months, patients with normal or euthyroid thyroid levels must have a thyroid function test because a sizable portion of them will experience thyroid abnormality within two years.
- Radioactive iodine therapy: In 24% of cases of TED, radioactive iodine therapy (RAIT) worsens the condition.
- Family history of TED: Inheriting a particular gene or a set of genes may increase a person’s risk for thyroid disorders or Graves’ disease.
- Age: A bimodal peak incidence is seen in TED. It affects people between the ages of 40 and 44 and 60 to 64 for women and between the ages of 45 and 49 and 65 to 69 for men. Patients who are older and more likely to have more severe thyroid eye disease.
- The onset of symptoms: Quick onset of symptoms in less than three months predisposes the patient to more severe ocular involvement.
- Chronic conditions: uncontrolled blood cholesterol levels and uncontrolled blood sugar levels in diabetes
- Peripheral vascular diseases
- Life stressors: Psychological stress can exacerbate TED.
- Gender: It is more common among women than men due to the higher risk of autoimmune diseases. The disease affects 16 out of every 100,000 female births and 2.9 out of every 100,000 male births, respectively. Male cases have worse outcomes and more severe ocular involvement.
Symptoms
Foreign body sensation in the eyes, photophobia, lacrimation, dry eye, discomfort, and forward eye protrusion (Proptosis).
In more severe conditions, the patient might experience pain in the eye socket, double vision, or blurred vision.
Ocular signs of TED:
Increased inflammation and consequent fibrosis of the ocular tissues cause the following ocular signs:
1. Eyelid retraction:
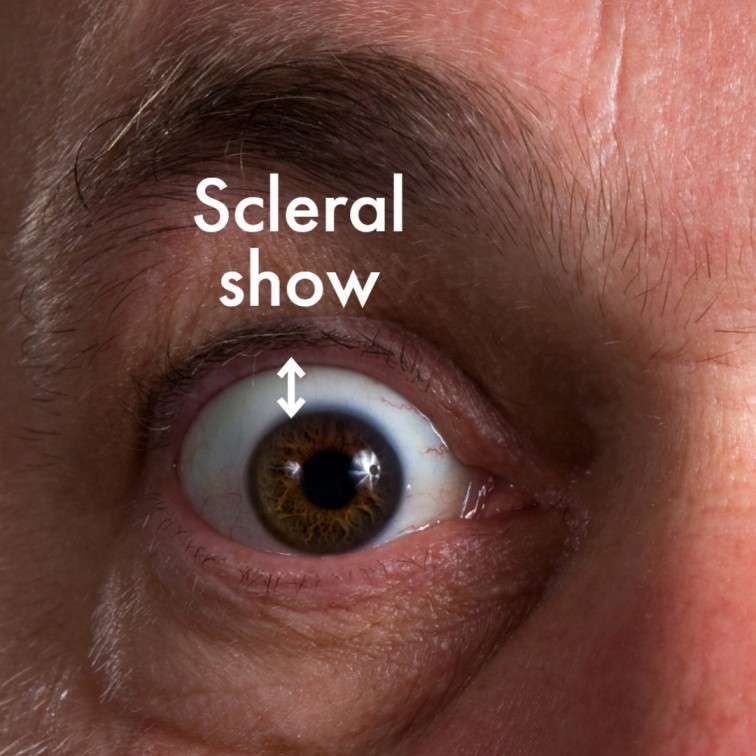
Eyelid retraction occurs in up to 90% of patients with TED. In TED, the upper eyelid is retracted, revealing more of the sclera than typical. Normally, an upper eyelid covers roughly 0.5 to 1.5 mm of the cornea.
Up to 49% of TED cases exhibit lower lid retraction.
Most TED patients (between 90 and 98%) exhibit upper lid retraction.
2. Lid lag

Von Graefe’s sign is the lagging of the upper eyelid on downward rotation of the eye.
2. Eyelid edema:

The enlarged extraocular muscles constrict the superior ophthalmic vein (SOV) in TED, causing venous stasis.
This venous congestion causes the conjunctiva and eyelids to swell and turn red.
3. Proptosis:

TED is the most common cause of unilateral or bilateral axial proptosis (exophthalmos) in adults. Increased swelling in the EOM causes the eye to protrude forward.
Exophthalmometers are used to measure the outward protrusion of the eye.
4. Exposure keratopathy:

Eyelid retraction and partial upper eyelid closure continuously expose the cornea and conjunctiva, causing dryness and corneal damage.
This is a significant contributing cause to the decreased visual acuity and impaired vision associated with TAO in addition to compressive optic neuropathy.
It tends to happen in 1-8% of cases. In extreme circumstances, the cornea may sustain damage that results in ulceration, perforation, infection inside the eye, or endophthalmitis, a potentially blinding condition.
5. Diplopia:
TAO frequently involves extraocular muscles. Affected extraocular muscles cause ocular misalignment and diplopia or double vision.
Most commonly, the inferior rectus muscle is involved, followed by the medial rectus muscle. As a result, patients have double vision or limited ability to look up and/or inward. Eyes are unable to converge due to the involvement of the medial muscle, which controls the eye’s inward movement, making near work challenging.
6. Superior limbic keratoconjunctivitis:
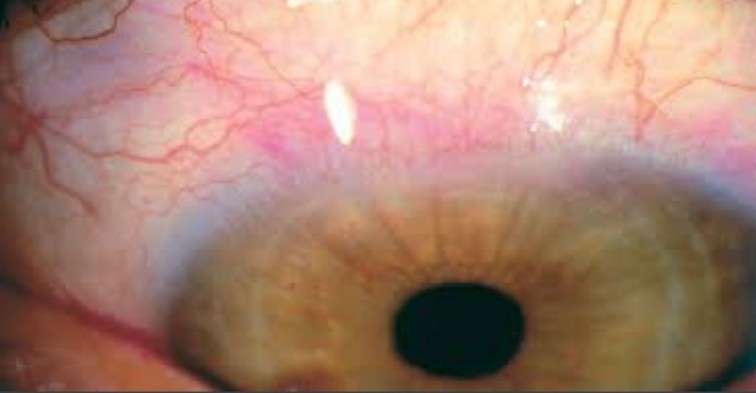
In 0.9% of patients, superior limbic keratoconjunctivitis (SLK) is present. Swelling and inflammation of the conjunctiva, as well as retracted eyelids, cause laxity of the conjunctiva, which causes friction when blinking, resulting in SLK.
7. Dry eye:
13-20% of patients experience dry eye symptoms and watering.
8. Optic neuropathy:
A 5% prevalence of patients with typical TED develops compressive optic neuropathy, an ocular emergency that causes visual loss over time.
The oversized extraocular muscles and orbital fat cause compartment syndrome at the apex of the orbit.
Reduced vision, color vision, contrast sensitivity, and a relative afferent papillary defect are its defining features.
Clinical pathway:
In TED, an inflammatory phase is followed by a stable post-inflammatory phase.
The Rundle’s curve, which plots the severity of orbital disease against time, describes the disease’s pattern.
Initial phase- inflammatory phase duration may range from 6 to 18 months, including proptosis and retraction of the orbit and periorbital region.
Static phase: gradual improvement and a decline in the inflammatory phase.
TESTS AND DIAGNOSIS
A physical eye examination by a medical professional will enable them to identify thyroid eye disease. Other tests include:
Blood tests:
Blood levels of Thyroid hormone levels, thyroid-stimulating immunoglobulins (TSI), and anti-thyroid antibodies can point to a diagnosis.
Ultrasound of the eyes.
An A-scan or B-scan transocular echogram can be used to visualize the orbital structures and the size of the eye muscles.
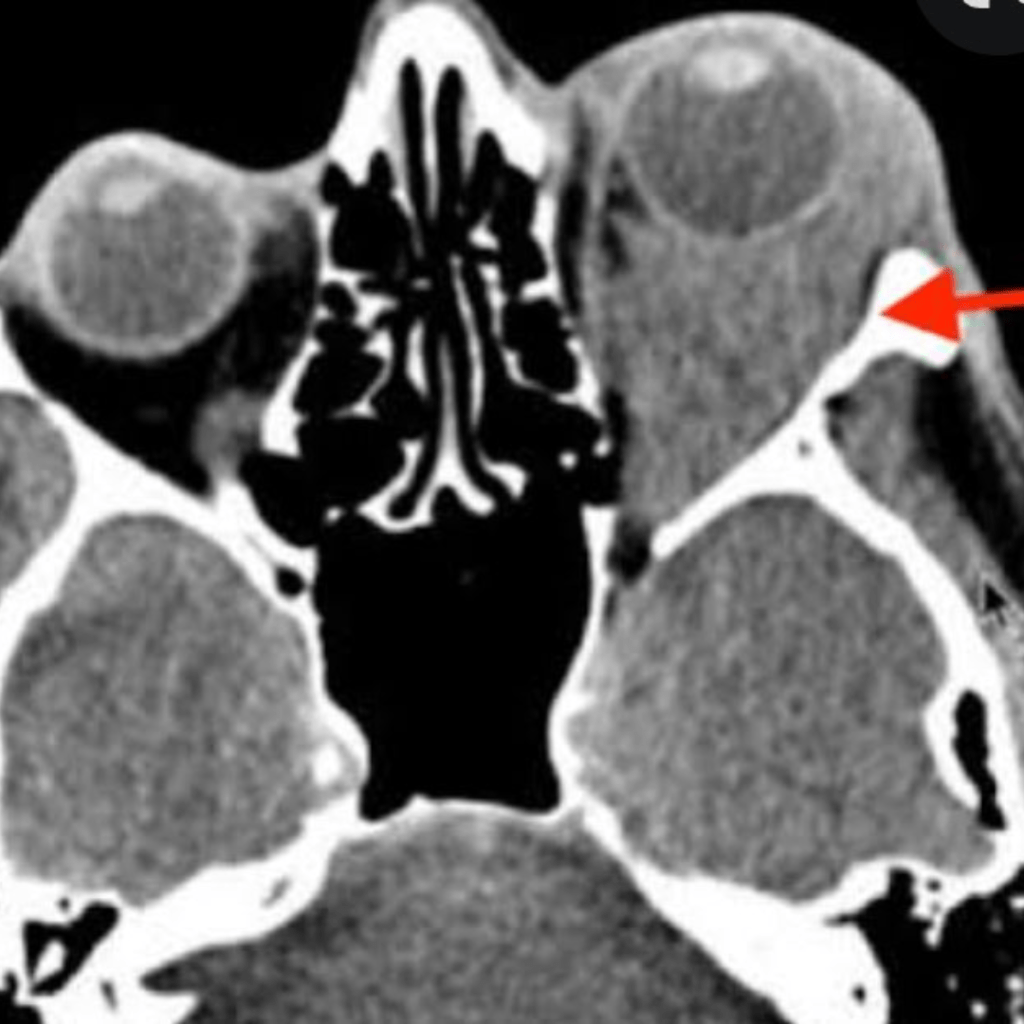
computed tomography (CT) scan
The optic nerve, an enlarged EOM, edema, and measurement of proptosis are all analyzed. It aids in determining how the optic nerve and muscles at the orbital apex relate to one another, assisting in the planning of any necessary surgical intervention.
MRI, or magnetic resonance imaging
In addition to viewing structures, this imaging modality can be used to assess disease activity and severity.
MANAGEMENT
The three types of management are conservative, medical, and surgical:
Conservative:
- Quit smoking
- Tape your eyelids shut at night: Lack of eye closure can cause dryness and corneal ulcers, which can leave scars on the eyes and impair vision.
- Apply eye lubricating drops for comfort and prevention of irritation and dryness.
- Limit sodium intake to lessen tissue edema and water retention.
- To lessen double vision, wear prism-equipped glasses.
- Reduce double vision by applying a patch to one eye.
- By adhering to your doctor’s advice and scheduling routine thyroid exams, you can maintain a healthy level of thyroid hormones.
MEDICAL THERAPY:
1. NSAIDs:
Periocular pain can be treated with anti-inflammatory medications taken orally.
2. Selenium:
In patients with mild, non-inflammatory orbitopathy, selenium has demonstrated a significant benefit by lessening the severity and progression.
3. Teprotumumab:
Clinical studies have demonstrated that the biological infusion therapy teprotumumab can lessen the signs and symptoms of TED.
The first and only TED prescription medication to receive FDA approval is Tepezza (Teprotumumab-trbw).
4. Systemic steroids:
Oral steroids may be administered for a maximum of two months to reduce orbital inflammation.
Patients with sight-threatening disease may benefit from intravenous glucocorticoids (IVGCs) as a short-term and urgent treatment for reducing disease activity. VIGCs may also be considered in moderate to severe cases of TED.
5. Radiation therapy:
In conjunction with corticosteroids or on its own, orbital radiation therapy can be applied as a modality during the acute inflammatory stage of TED or as a way to slow down the disease’s progression and provide long-term control.
It generally improves double vision caused by restrictive eye muscles.
SURGICAL:
1. Orbital decompression:
This procedure enlarges the eye socket by removing some of the bony walls and occasionally fat, which relieves pressure on the optic nerve. Typically, the orbital floor, medial wall, and lateral wall are all involved in orbital decompression. Rarely, it may also be necessary to perform surgery on the orbital roof.
2. Surgery for strabismus:
In cases of severe strabismus, surgery may be necessary. Only after orbital decompression surgery and stable muscle alignment should strabismus surgery be considered.
3. Surgery for eyelid retraction and tarsorrhaphy:
Tight eyelids prevent bottom lid from rising and top lid from descending. This might harm the cornea.
These reconstructive surgical procedures can be used to treat exposure keratitis or eyelid retraction.
SHORT SUMMARY:
Anyone can develop thyroid eye disease, but Graves disease or a thyroid condition increases the risk. If you notice that your vision is blurry or that your eyes are frequently watery, dry, or gritty, get in touch with your healthcare provider. Early detection and treatment of thyroid eye disease are crucial to minimizing any potential harm.

