Treatment with steroids is effective for inflammatory and immune disorders, but long-term or high-dose use is associated with unfavorable side effects. Therefore, it is necessary to keep an eye out for any adverse effects. The main concern is educating individuals to avoid abusing the medicine by purchasing it over the counter or taking it carelessly and unsupervised.
Ophthalmology uses both local (eye drops, subconjunctival, and intravitreal applications) and systemic treatment modalities.
A thorough medical examination is performed prior to starting steroid eye drops in order to identify potential risk factors (for example, bronchial asthma, diabetes, etc.).
Uses for Ophthalmic Steroids
1. Allergic or noninfectious conjunctivitis:

Topical corticosteroids with gradual tapering of the dose is recommended for patients with ocular allergies who have not responded to two to three weeks of antiallergy medication.
Extended use of high-potency steroids can cause glaucoma if unsupervised and improperly handled.
2. Acute anterior and chronic posterior uveitis:
The treatment of anterior uveitis is typically local; however, periocular or systemic treatment is usually necessary for patients with more severe or posterior uveitis involving the retina, choroid or vitreous.
3. Post keratoplasty:
The gold standard for preventing rejection after corneal transplantation is the use of topical corticosteroids. Due to its immunosuppressive properties, long-term, low-dose topical steroid treatment prevents immune graft rejections.
4. Giant cell arteritis:
Intensive systemic therapy for giant cell arteritis can prevent blindness.
5. Post-trauma or surgery:
Steroids are commonly prescribed following trauma or surgery to reduce inflamamtion and vascularization.
6. Optic neuritis:
Intravenous methylprednisolone, followed by oral prednisone, hastens the recovery of vision loss as a result of optic neuritis and yields marginally better vision at six months.
7. Thyroid eye disease:
The anti-inflammatory and immunosuppressive properties of glucocorticoids make them an effective method for medical decompression in thyroid orbitopathy.
The treatment of TED frequently uses oral glucocorticoids, despite their side effects.
Intravenous glucocorticoid (IVGC) is a short-term and urgent treatment used to reduce disease activity in individuals with the sight-threatening condition and sometimes in active moderate to severe TED.
RISK FACTORS:
The following history should be obtained since these patients have an increased risk of complications.
- Cataracts,
- Glaucoma,
- Hypertension,
- Diabetes,
- Hyperlipidemia,
- Renal stones,
- Peptic ulceration,
- Current infection or
- Pregnancy
DANGERS:
There are various ways in which anti-inflammatory steroids can affect your eyes and vision. Generally speaking, side effects are more probable the longer you take them or the higher the dose.
According to the American Academy of Ophthalmology, taking lower doses of steroids for a longer period of time is more likely to result in cataracts than taking higher doses of steroids followed by a tapering off period.
1. Glaucoma:

Eyes receiving corticosteroids should always have their intraocular pressure checked. Prior to treatment, a baseline intraocular pressure reading is recommended, and then regular readings should be performed, first every few weeks and then every few months.
It usually takes 4-6 weeks for the ocular response to a steroid-induced rise in intraocular pressure to show (steroid-responder), and the effect fades after stopping therapy.

It is more common for topical steroids to cause glaucoma than systemic steroids.
Intraocular pressure can rise as a result of steroid therapy, particularly when administered for an extended period.
The use of topical ocular corticosteroids puts infants at a higher risk of developing systemic toxicity. Because newborns and infants have thin eye membranes, drug absorption and corneal permeation may occur more quickly in these populations, resulting in systemic side effects.
2. Cataract:
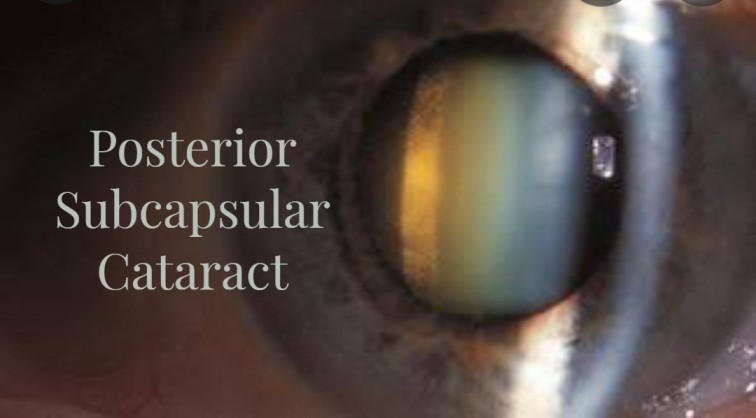
Steroid treatment for eye conditions may result in the development of posterior subcapsular cataracts, which are dose-dependent lens opacities.
However, ocular inflammation itself has the potential to cause opacities. This tendency will increase with steroid therapy.
Screening with a slit-lamp exam can detect cataracts, which can arise from continuous use of systemic steroids.
Intermittent topical and systemic steroid users should have these exams twice a year; long-term patients should have them three or four times a year.
3. Opportunistic ocular infections
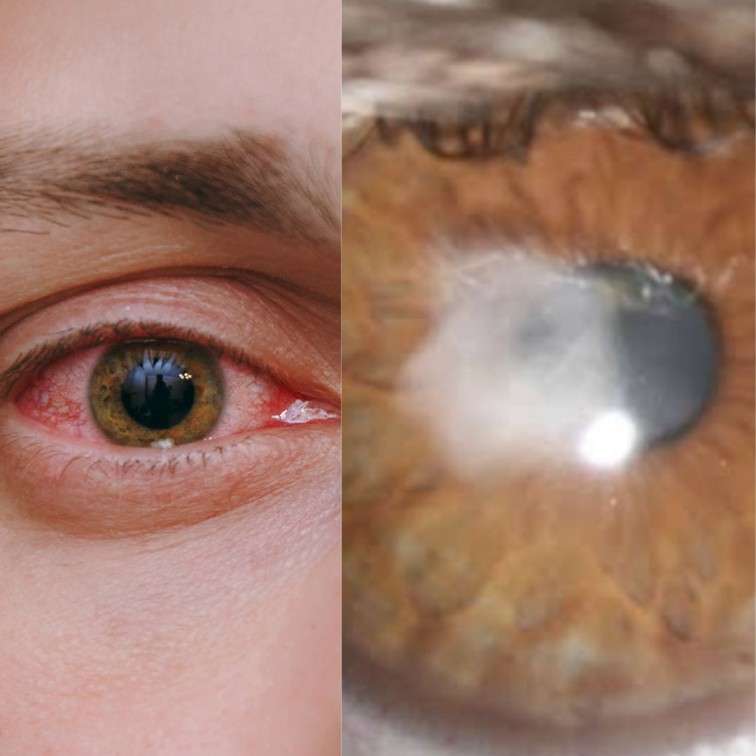
When steroids are used to treat ocular conditions, they induce immunosuppression, which can lead to the development of bacterial, viral, or fungal eye infections.
Infections with fungi are especially susceptible to growth. The disastrous impact of steroids on herpetic epithelial keratitis and the enhanced herpes simplex keratitis caused by unsupervised local steroid use is of the utmost practical significance.
Patients receiving ocular steroids should seek immediate ophthalmologic evaluation if they experience ocular discharge, pain, photophobia, or redness.
4. Ocular rebound inflammation:
Ocular rebound inflammation may appear after abruptly stopping the use of topical ocular steroids or rapidly tapering off the dosage.
Even though the disease may have been dormant for a considerable amount of time, attempts to reduce the dose in patients who have grown accustomed to it over many months or years frequently result in a flare-up.
Once control has been achieved, the lowest effective dose should be sought, and the reduction should be gradual and closely monitored.
HOW TO REDUCE SYSTEMIC ABSORPTION:
The systemic absorption of steroids, even when prescribed as eye drops, can occasionally result in adverse effects
A few simple rules can greatly reduce the systemic absorption of drugs from eye drops.

- Not more than one drop should be applied to the conjunctival sac of the eye.
- After putting the drop, either gently close your eyes for a couple of minutes or do digital nasolacrimal occlusion for a few minutes. To do this, lightly press your clean finger over the tear duct located in the inner corner of your eye, close to your nose.
Conclusion:
One should not self-medicate with corticosteroids, but only obtain them from a medical professional with access to a slit lamp and intraocular pressure measurement tools.
In order to avoid the misuse of steroids, patients, ophthalmologists, and the government must work together.
With extraordinary benefits against various eye illnesses, the steroid is a double-edged sword. It is important to watch out for signs of systemic toxicity, especially in pediatric patients and newborns on topical steroid drops, as they are particularly susceptible to it.
