Keratoconus is a progressive eye condition that affects the cornea, the outermost transparent window of the eye. The disease causes the cornea to thin and bulge outward due to a weakening of its stromal layer. While both eyes can be affected, the symptoms may be more severe in one eye.
ETIOLOGY:
The exact cause of keratoconus is not known, but it is believed to be related to the degradation of collagen fibers in the cornea caused by enzymes. This process is exacerbated by eye rubbing, which can cause mechanical trauma in those who are genetically predisposed. To prevent progression of the disease, it’s important to effectively treat eye allergies and minimize eye rubbing.
Keratoconus is also associated with conditions such as Down’s syndrome, Ehlers-Danlos syndrome, hay fever, and connective tissue diseases. The incidence of keratoconus in individuals with Down’s syndrome can range from 0.5% to 15%.
SYMPTOMS:
Frequent change in glasses or contact lens prescription
Image distortion, and
Increased sensitivity to glare and light.
NATURAL COURSE OF PROGRESSION OF KERATOCONUS:
When the disease progresses, spectacles are unable to compensate for the loss of visual acuity.
Keratoconus (KCN) may manifest clinically during puberty (late teens for males and early twenties for females) and progress (continuous stromal thinning and corneal steepening) until the third or fourth decade.
Usually, no progression occurs after this age. It is possible for KCN to manifest at a later age, following an alteration in the endocrinologic status such as pregnancy or gestation.
Evaluation
Diagnosing Keratoconus (KCN) requires a comprehensive eye exam. The two most telling signs of KCN are irregular corneal astigmatism and a thinning of the cornea’s stromal layer. A doctor may look for the following during an examination:

- Irregular Astigmatism: Difficulty in correcting vision with glasses may indicate KCN, even in mild cases. Corneal topography can also reveal early signs.
- Munson’s Sign: Advanced KCN is characterized by a v-shaped protrusion of the lower eyelid on downward gaze.
- Scissoring Reflex on Retinoscopy: In a retinoscopy examination, the doctor shines a light into the patient’s eye and assesses the reflection of light from the retina. In a healthy eye, the reflection of light will be a single streak, but in a keratoconic eye, the reflection may split into two separate streaks due to the irregular shape of the cornea. This splitting of the light is called scissoring reflex and is a characteristic sign of keratoconus.
- Slit Lamp Signs: During a slit lamp exam, the doctor may look for Vogt’s striae (fine vertical stress lines), Fleischer ring (deposition of iron at the base of the conical protrusion), corneal thinning, corneal apical scarring, and hydrops (swelling caused by the imbibition of fluid into the cornea).
It’s essential to seek treatment if you suspect you may have KCN, as it is a progressive disease that may lead to vision loss
CORNEAL TOPOGRAPHY
Keratoconus (KCN) is diagnosed through comprehensive eye exams and diagnostic tests. One of the most important tests for KCN is corneal topography, also known as PENTACAM.
Corneal Topography (PENTACAM): A visual representation of the irregularity on both the front and back surfaces, curvature, and thickness of the cornea is created by using a rotating camera. The test results in four colored maps:
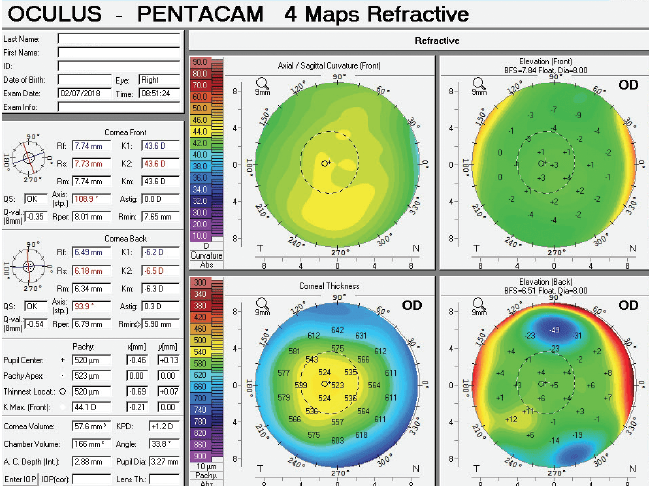
- Curvature Map: Measures the steepness at each point on the curve.
- Anterior Elevation Map: Shows the difference in elevation between the patient’s front cornea and a reference body.
- Posterior Elevation Map: Shows the difference in elevation between the patient’s back cornea and a reference body.
- Pachymetry: A corneal thickness map that shows thinning in the inferotemporal region, which is typical of KCN.
Other diagnostic tests for KCN include:
- Tear fluid as a biomarker
- Corneal biomechanics
These tests help confirm the diagnosis of KCN, even in cases of subclinical keratoconus
Treatment / Management
There is no cure for keratoconus. Patients with progressing keratoconus are treated with the goal of stopping the progression, while those with stable corneas are treated with the goal of providing the best visual results.
STOPPING THE PROGRESSION:
Corneal collagen crosslinking with riboflavin (C3R or CXL)
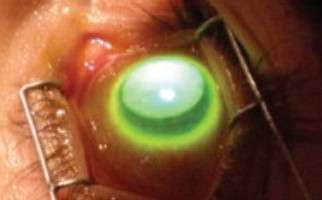
Keratoconus is a condition that causes the cornea to thin and bulge, leading to vision loss. C3R/CXL is a procedure that halts the progression of keratoconus and prevents future vision loss in patients diagnosed and treated early. FDA approved C3R/CXL in April 2016.
Different Types of C3R/CXL
For Patients with Corneal Thickness >400 Microns:
- Dresden Protocol
- Accelerated CXL
In Dresden Protocol, the epithelium is debrided, the stroma is soaked in riboflavin for 30 minutes and then exposed to 3 mW/cm2 of UVA light for 30 minutes. Accelerated CXL shortens the treatment time by increasing the power of UVA irradiance – 5 minutes at 18 mW/cm2 or 10 minutes at 9 mW/cm2. A study showed better topographic improvements with 10 minutes of UVA at 9 mW/cm2.
For Patients with Corneal Thickness <400 Microns:
- Epi-on C3R/CXL
- Contact Lens Assisted C3R/CXL
- Iontophoresis for Riboflavin (I-CXL)
- Lenticule Induced C3R/CXL
Options for patients with a thin cornea include keeping the epithelium intact (Epi-on C3R/CXL), using a soft contact lens during the procedure (Contact Lens Assisted C3R/CXL), applying an electric current to enhance the penetration of riboflavin (I-CXL), and using SMILE lenticules (Lenticule Induced C3R/CXL).
C3R/CXL also has the potential to be combined with topography-guided laser-ablation (Athens protocol) for improved visual function.
VISION CORRECTION:
RGP lenses and scleral contact lenses:
For patients with Keratoconus, spectacles and spherical/toric soft contact lenses can only provide limited vision correction. The primary method for achieving better vision correction in modest to advanced stages of KCN are Rigid Gas Permeable (RGP) or scleral contact lenses.
RGP lenses have the advantage of creating a tear pool between the lens and the cornea, which helps eliminate certain visual aberrations associated with KCN. However, they also come with challenges such as difficulty wearing, intolerance, and potential for allergic reactions, corneal abrasions, and new blood vessel growth.
For those who face difficulties with RGP lenses, alternatives such as hydrogel contact lenses, piggyback contact lenses, and scleral contact lenses are also available for vision correction in KCN
INTACS:
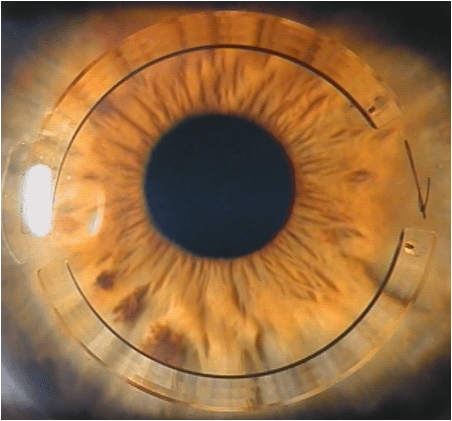
These are semi-circular PMMA rings implanted within layers of the cornea surrounding the cone to flatten its center and to provide smooth and regular surface. This is done with an effort to improve vision in stable KCN.
Corneal transplant:
When the cornea is too thin for CXL and the symptoms are severe, corneal transplant is considered the last resort. The corneal transplant in keratoconus is quite successful with 90-95% success rate. The cornea is replaced either fully (penetrating keratoplasty) or partially (Lamellar keratoplasty).
QUICK SUMMARY
The cornea of a person with KCN becomes weaker and starts protruding outward as they age. Managing the condition is about stopping the progression and offering the best vision correction option. By timely diagnosis and C3R treatment, the progression can be halted. Vision correction options include RGP and scleral contact lenses, topography-guided c3r, Intacs and optical keratoplasty as the last resort.
