A glaucoma is a group of diseases causing progressive damage to the sight which finally leads to irreversible blindness.
In many cases it is painless and affects the peripheral vision first, therefore people having glaucoma may not even realize that they have it until it’s too late.
There is a growing need to help people understand how important an annual routine eye examination by a trained eye physician is. Glaucoma, like many other eye diseases, can be treated early and monitored regularly, thus preserving the vision that is left.
Glaucoma is the leading cause of blindness in patients more than 60 years of age.
In glaucoma, the nerve in the eye called the optic nerve, which connects the back of the eye to the brain, is damaged, usually due to increased pressure in the eyes.
There is no cure for glaucoma, but treatment can help reduce the pressure and halt its progression.
What causes Glaucoma?
Just like there is pressure in our blood vessels known as blood pressure, there is pressure in our eyes called intraocular pressure.
Glaucoma is usually caused by raised intraocular pressure or IOP. This raised IOP compresses the optic nerve at the back of the eye which leads to irreversible loss of vision.
How is IOP maintained in the eye?
IOP is maintained by a fluid called aqueous humor that is constantly made and drained by the eyes.
The newly secreted aqueous humor feeds the various eye structures while the old aqueous humor collects waste.
The waste exits the eyes and enters the bloodstream through a drain-like structure called the trabecular meshwork, which is situated at the drainage angle.
This equilibrium maintains the eye pressure.
Types of glaucoma:
It is important to know what type of glaucoma one has, as it determines which treatment modality to go for. Some of the types are
1. Primary open-angle glaucoma or POAG: This is the most common type of glaucoma. Here the trabecular meshwork gradually becomes less effective at draining the fluid hence there is a build-up of fluid in the eyes, causing the IOP to rise, which puts pressure on the optic nerve.
2. Primary angle-closure glaucoma or PACG: Here the drainage angle becomes narrow and the fluid gets accumulated behind it, putting back pressure on the optic nerve.
3. Normal-tension glaucoma: According to the available testing, the IOP and drainage angle are both normal in this case, yet the optic nerve is nonetheless damaged.
Possible causes:
- Normally the IOP fluctuates throughout the day but is usually in the range of 3-6 mm of Hg. Fluctuations of 8-30mm of Hg are seen in untreated glaucoma patients.
NTG patients may have normal pressure throughout the day but there can be marked nocturnal IOP spikes.
- As the IOP measurement depends on corneal rigidity or how rigid the outer layer of the eye is, some patients with thicker corneas show falsely high IOP, and patients with thin corneas can show falsely low IOP.
Therefore patients with thin corneas can still have glaucoma even if the IOP measurement is normal.
4. Secondary open-angle glaucoma: Here, the trabecular meshwork gets clogged with debris (similar to how your bathroom floor drain might occasionally be blocked with hair), which raises eye pressure and harms the optic nerve.
This condition is called secondary open-angle glaucoma. The debris can be made of inflammatory cells, pigments (pigmentary glaucoma), dandruff-like particles (pseudoexfoliation glaucoma), etc
5. Secondary angle-closure glaucoma: Imagine your bathroom drain is covered with a block of wood. The holes are not closed; rather, an obstruction or a wooden block has been placed over them to prevent water from draining.
When it comes to the eyes, the obstruction may be caused by abnormal blood vessels or a swelled-up lens, abnormal cells migrating from the cornea, tumors, etc. This is known as secondary angle-closure glaucoma.
6. Congenital glaucoma: This type of glaucoma is present since birth. The cause is a defect in the drainage angle, which prevents or slows aqueous outflow, thus building pressure inside the eyes. Children born with congenital glaucoma usually have enlarged eyes, hazy corneas or cloudy eyes, excessive tearing, and increased sensitivity to light or photophobia.
symptoms
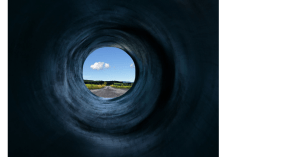
Open-angle usually doesn’t have any symptoms and is noticed by the patient only when the visual field starts to get affected. Therefore glaucoma is sometimes referred to as the ‘silent thief of sight.
The vision once gone cannot be brought back and since it is symptomless, the disease is detected much later. Therefore a regular eye checkup is very important.
Angle-closure glaucoma: This is an ocular emergency wherein the IOP rises rapidly and there is an immediate need to bring the pressure down.
The symptoms include:
- Sudden loss of vision
- Severe pain in and around eyes along with headache
- Nausea and vomiting (secondary to severe pain)
- Rings or halos around light
DIAGNOSIS
Glaucoma can be diagnosed using the following methods.
1. Routine slit lamp examination: The doctor can pick up subtle optic nerve findings suggesting glaucoma.
2. IOP measurement: IOP is the only modifiable risk factor in glaucoma and is easily measured using an instrument called a tonometer.
In patients with NTG, the IOP is recorded in the hospital for over 8 hours during office hours. Sometimes patients are kept in the hospital for 24 hours and 4 hourly measurements of IOP are done to see if there are any unusual spikes in IOP, especially at night.
3. Perimetry: This measures the field and depth of vision that are affected in glaucoma.

Visual field testing at an early stage can help prevent further visual field loss.
4. Pachymetry: It measures the thickness of the cornea. Thick corneas can often show falsely elevated IOP while thin corneas can falsely give low IOP readings.
Therefore a person with thin corneas but IOP in the normal range can still have glaucoma.
5. Ocular ultrasound in angle closure to see the structures blocking the mesh.
6. OCT /RNFL: It is to document the damage to the optic nerve and surrounding structure.
7. Gonioscopy: It’s a lens kept in front of the patient’s eyes to visualize the angle through the microscope.
Who can have glaucoma?
There are various risk factors to consider
- Age above 40
- Family history of glaucoma
- Race: African, Hispanic, or Asian
- Refractive errors such as myopia (susceptible to open-angle glaucoma), hypermetropia (angle-closure)
- History of eye trauma or surgery
- Long-term steroid medications
- High IOP
- Thin corneas
- Certain findings in the optic nerve
- Constricted visual field
Medical history of diabetes, hypertension, migraines, etc.
How is it cured?
Once damaged, the fine fibers of the cable can not be replaced or regenerated so treatment is aimed at preventing/delaying further loss of these fibers. This can be done by medications, laser procedures, or surgery.
Medications:
The medications are given either to reduce the production of aqueous humor or increase its evacuation through the drainage channels. Once prescribed by your ophthalmologist, these have to be used regularly and diligently. Make sure you are going for your regular follow-ups.
Many times after doing some tests, your ophthalmologist may decide to add another drug, change a drug or even put you on a low-dose one. The treatment needs to be gauged regularly. Therefore compliance and regular follow-up are very important.
These medications are mainly eye drops and therefore as a side effect can have redness, irritation, itching, stinging, blurring, or even cause a change in the eye color and thickening of eyelashes.
Laser Procedures
Laser procedures are outpatient procedures done in a doctor’s office. The eye is numbed by an anesthetic eye drop and a laser is applied to the eye. Laser treatment helps in some types of glaucoma and may be required more than once.
1. Peripheral iridotomy: This is a procedure in which a laser is applied to the eye to create a full-thickness hole in the peripheral iris in patients with narrow angles (at risk for angle-closure). This opening creates an alternative path for the aqueous humor to flow.
2. Laser trabeculoplasty (argon or selective) can be used to tighten the trabecular meshwork, which in turn opens some drainage channels, which enhances the aqueous flow. This is done in open-angle glaucoma.
When is Surgery indicated?
Indications for surgery include conditions such as:
1. IOP not coming down even after maximum medical therapy.
2. The patient is not compliant with the medication or follow-up/ or it’s not possible to follow up regularly.
3. Intolerable side effects with topical medications.
4. The patient opts for surgery instead of lifelong medication.
Surgery
Surgery cannot reverse vision loss or cure glaucoma but it helps alter the anatomy of the eye to help with aqueous drainage, thus keeping the IOP down and preventing further damage to the nerve.
Glaucoma surgery has a success rate of 70-90% in the first year of surgery but some post-operative procedures or medication may be required during follow-up to maintain the IOP.
1. Goniotomy: This is a pediatric glaucoma surgery done for primary congenital glaucoma. The surgeon uses a gonio prism to visualize the drainage angle and an instrument is used to remove the obstruction(membrane) from the trabecular meshwork, thus enhancing the aqueous outflow.
2. Penetrating filtering surgery/ trabeculectomy: Trabeculectomy can be broken down into trabecular as in trabecular meshwork, and ectomy or “to excise”. So this means that a piece of the trabecular meshwork is excised and a new pathway is created for the aqueous humor to flow out of the eye.
This procedure involves the creation of a space in the subconjunctival area where the fluid is collected and later drained into the blood circulation. An elevation of the conjunctiva, known as a filtering bleb, typically results from the aqueous flowing into this subconjunctival space.
3. Non-penetrating filtering surgery: The popular method in this category is Canaloplasty. It is a procedure wherein a suture, with the help of a microcatheter, is threaded 360 degrees through the drainage canal to enlarge it.
Unlike in traditional filtering surgery, here there is no excision and no bleb formation.
4. MIGS (Minimally invasive glaucoma surgery): This procedure is for patients with open-angle glaucoma, which aims to enhance patients’ drainage system by bypassing the resistance in the drainage pathway, either by placing an implant (istent, Hydrus) within the pathway or by a popular procedure called GATT (Gonioscopy-Assisted Transluminal Trabeculotomy).
GATT is a minimally invasive surgical treatment in which a goniolens is used to identify the angle structures and a small incision is made in the drainage canal.
A microcatheter is then passed through the opening and is threaded 360 degrees throughout the circumference of the drainage canal.
It is then pulled towards the center leading to the ripping off of the trabecular meshwork, which lies near the drainage canal.
This reduces the resistance and enhances the aqueous outflow through the drainage angle.
Minimally invasive endoscopic laser procedure is the other method in this category to reduce the production of fluid by ablating the aqueous secreting structure.
MIGS is a bleb-free surgery therefore bleb related complications are not present.
5. Artificial drainage devices or glaucoma implants: These consists of a drainage implant and a tube. The drainage implant is placed onto the sclera or white part of the eye, usually under the upper or lower eyelid.
A tube is attached to the implant and is inserted into the eye in front of the iris.
The fluid then passes through this tube and gets collected around the drainage implant from where it gets drained by the blood vessels.
6. Cyclodestructive procedure: Cyclodestruction is usually the last resort in the treatment of glaucoma. It is indicated in painful eyes, commonly with poor visual acuity or poor visual potential.
First, an anesthetic injection is given near the eyeball to reduce pain and movement, and then the laser is applied with a probe 360 degrees around the junction between the outermost transparent layer (cornea) and white (sclera) part of the eye known as limbus.
Underneath the limbus is the structure that is responsible to produce fluid in the eye therefore by ablating these structures, the production and secretion of aqueous humor are reduced, thereby reducing the IOP.
A Quick Summary
Glaucoma is one of the leading causes of blindness worldwide. The high eye pressure in glaucoma causes damage to the optic nerve resulting in loss of vision.
This loss is irreversible and therefore a timely diagnosis and management is the key to stopping its progression and maintaining the vision. Therefore a routine eye examination is important.
Glaucoma cannot be cured but the progression can be halted by medications, lasers, or surgery. So discuss with your doctor the various treatment modalities and the best option for you.
If you have any doubts or queries regarding this topic, please feel free to drop us a message.
Disclaimer: The content on this site is for general information only and should not be used as a substitute for professional medical advice.



