The retina can become detached from the back of the eye in a condition known as retinal detachment.
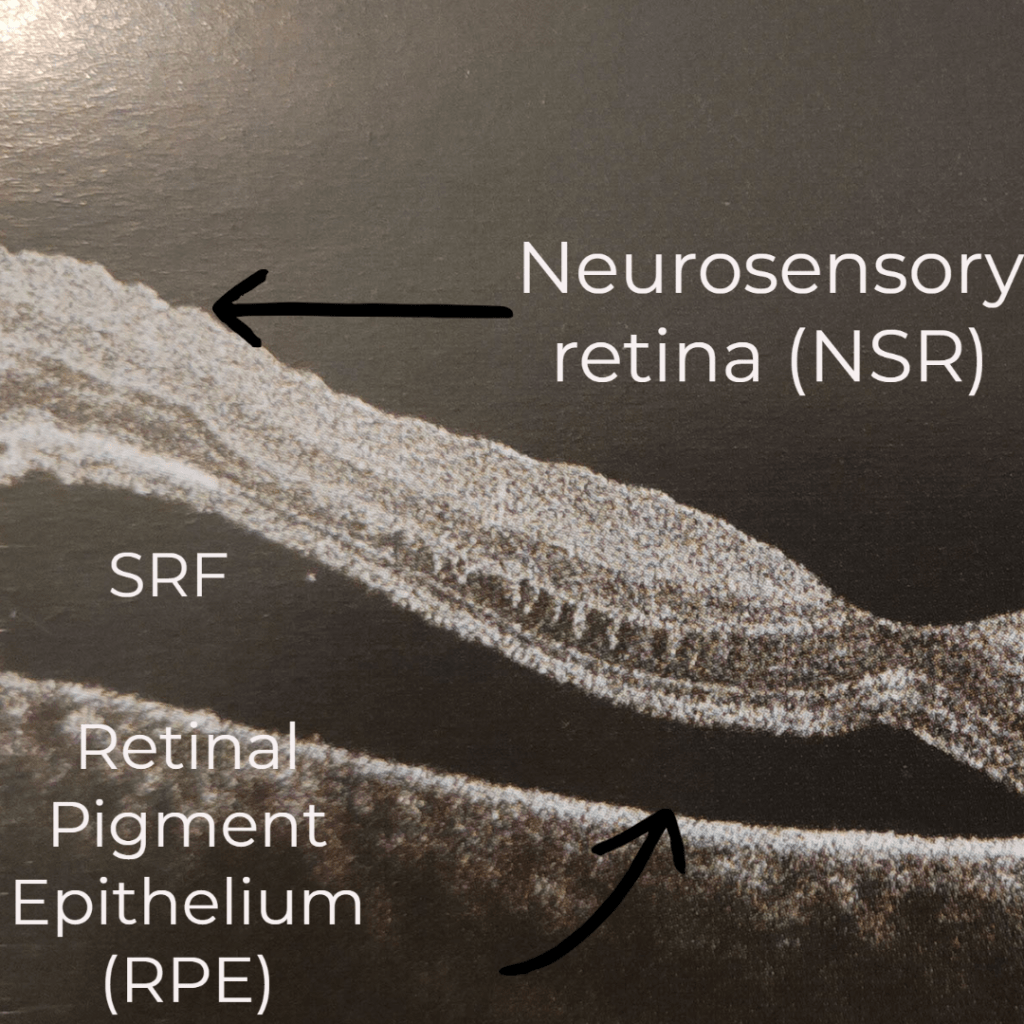
The retina can be divided into two sections to better understand retinal detachment:
- The RPE layer, which has the pumping action that expels all of the waste material and,
- The neurosensory retina (NSR) consists of photoreceptors, bipolar cells, and ganglion cells, which contribute to vision and perception.
There is a potential gap between the RPE and NSR called the subretinal space.
There can be a buildup of fluid in this space (sub retinal fluid), more than the RPE can pump out, which causes swelling in this area and eventually retinal detachment.
TYPES OF RETINAL DETACHMENT
Retinal detachment can be divided into 3 types according to the pathophysiology:
Rhegmatogenous
Tractional
Exudative
HOW THE TEAR FORMS:
Let’s first gain a basic understanding of the vitreous.
Approximately two-thirds of the eye is made up of a colourless jelly called vitreous which fills the posterior compartment behind the lens and in front of the retina. With a small amount of collagen fibres and other substances, this is 98 percent water.
Vitreous and retina are loosely attached, and the vitreous deteriorates with age or under certain pathological conditions, developing liquid-filled pockets.
Gradually, the vitreous separates from its connections to the back of the retina. After separation, the vitreous mass is only attached to the retina in the front of the eye.
The liquified vitreous moves in the opposite direction as the eye, so every time the eye moves, the vitreous pulls the retina along with it. The pull is usually without charge. Sometimes when it pulls, it makes a hole in the retina.
Liquified vitreous enters the hole, and as more fluid accumulates in the subretinal space, the detachment grows in size. The detachment will progress if not treated on time leading to vision loss.
Pathophysiology:
Rhegmatogenous RETINAL DETACHMENT (RRD):
This kind of RD begins as a tear. The vitreous can seep into the potential space because of the retinal tear. People who are susceptible to retinal tears include:
- Trauma
- History of retinal detachment in one eye
- Previous intraocular surgery such as cataract
- Pathological myopia (>6D)
- Anatomical irregularities such as Lattice degeneration, peripheral retinal excavations etc.
- Posterior vitreous detachment
Tractional RETINAL DETACHMENT (TRD)
The detachment occurs when fibrovascular tissue, such as new vessels in Proliferative Diabetic Retinopathy, pulls the retina away from the underlying structures. TRD may also result from the following additional factors:
- Trauma
- Retinal vein occlusion
- Retinopathy of prematurity
- Sickle cell trait or anemia
- Toxocariasis
Exudative/SEROUS RETINAL DETACHMENT:
This type occurs as a result of inflammation and SRF buildup beneath the retina, which pulls the retina away from the underlying layers. The fluid’s origin could be
- Ocular cancers
- Metastasis in eye
- Infection: syphilis, tuberculosis, toxocariasis
- Inflammation: posterior scleritis, VKH, Sympathelic ophthalmitis
- Vascular: wet AMD, malignant hypertension, preeclampsis
SYMPTOMS AND SIGNS:
- Sudden, painless vision loss
- Curtain-like or veil-like shadow in the VF
- Sudden flashes
- An abrupt rise in the number of floaters
People must schedule an eye exam immediately if they notice any of these sudden symptoms. The doctor examines eye to look for signs such as:
- Abnormal pupillary reflexes (RAPD)
- Pigments in the front and back of the eye
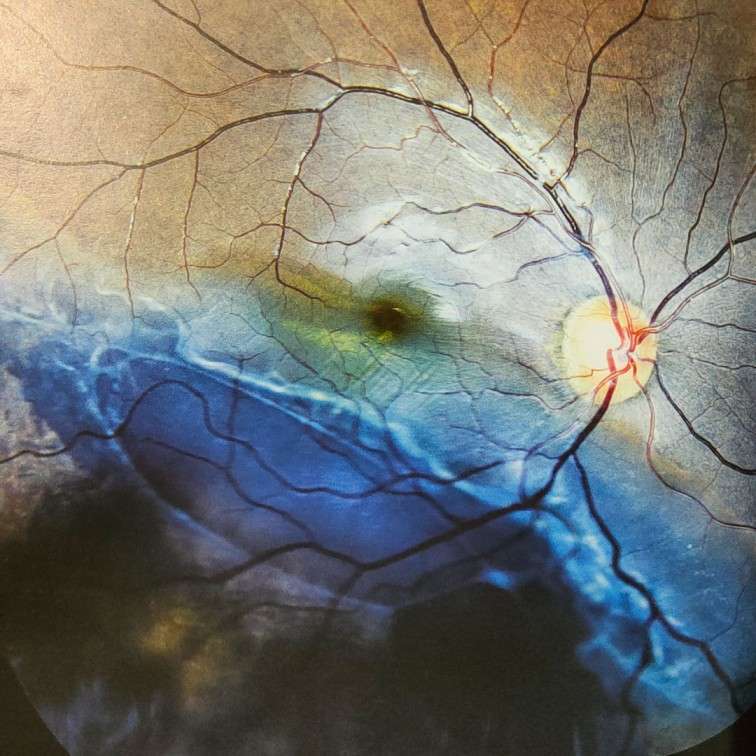
- Dilated fundus examination to locate the tear
- B scan or an eye ultrasound to assess the health of the retina in case of bleeding due to rupture of a blood vessel making it hard to examine.
TREATMENT OF RHEGMATOGENOUS RETINAL DETACHMENT:
TEAR WITHOUT RETINAL DETACHMENT:
Within 24 hours, patients with an acute retinal break must receive laser therapy or cryotherapy. The patient is then reexamined after two weeks, six weeks, three months, and then every six to twelve months.
Those without tears but with risk factors are monitored every three months and then every six to twelve months after that.
TEAR WITH RETINAL DETACHMENT:
Treatment focuses on dealing with the following three issues:
- Subretinal fluid accumulation between the RPE and NSR
- Pulling of vitreous on the tear
- Retinal tear
Currently, there are three treatment options for treating RRD:
- Pneumatic retinopaexy
- Scleral buckle
- Pars plana vitrectomy
PNEUMATIC RETINOPEXY:
Typically, this procedure is performed in a superior tear (8 to 4 o clock). The procedure involves injecting gas into the retina to temporarily seal the break. This gives the RPE time to pump the fluid out of the space.
It is important to follow the retina surgeon’s recommendations regarding head posture because the gas has a tendency to rise up. It is advisable to avoid flying during this time.
SCLERAL BUCKLE:
The procedure involves making an external incision after identifying the break in order to drain fluid and remove the SRF.
The following step involves burning the surrounding retinal tissue with a laser or freezing probe, which creates scarring around the tear and stops fluid leakage.
A band or buckle typically made of silicone is passed under the eye muscles and tightened around the equator.
The refractive change is this procedure’s main drawback. The buckle tightening results in the eye’s elongation, which leads to nearsightedness. A size change of even 1 mm can result in a 2.5–3D refractive change.
Additionally, there may be issues with eye mobility and an infection risk with the buckle.
PPV (Pars Plana Vitrectomy)
In PPV the entire vitreous is cut and removed. Additionally, PPV permits easy access to SRF, giving the choice to internally drain it.
Next, the retinal tissue near the breaks is lasered or frozen with a cryoprobe.
Injection of a gas bubble pushes against the retina to keep the break closed. For at least a week, the head position must be maintained. Depending on where the tear is and where the gas bubble should be, the person may be lying face down, propped up, or on the side. The retina surgeon will recommend this.
