Diwali is a festival of light, and lighting fireworks is an important part of the celebration. Unfortunately, during Diwali, the risk of firecracker injury increases significantly in India. It is one of the causes of ocular trauma threatening vision.
Children and young adults are at risk for irreversible blindness and ocular morbidity due to ocular trauma, and fireworks injuries account for 20% of all ocular trauma.
Vision damage from fireworks can be severe and permanently disabling. As a result, it’s critical to be aware of its risks, maintain a safe distance, and take other precautions to avoid having a bad accident.
EYE INJURIES DUE TO FIRECRACKERS
A research that examined hospital-based case studies of patients who suffered ocular injuries from fireworks between the years of 2017 and 2020 found that most of the cases involved males in their early 20s and children.

Lack of safety glasses, parental oversight, and close proximity to fireworks are risk factors for ocular trauma. Injuries to bystanders made up about 60% of the total.
The most frequent wounds were hyphema, superficial corneal and conjunctival foreign bodies, lid injuries, and corneal abrasions.
Few of these patients also had posterior segment injuries, the most frequent of which was retinal detachment, followed by vitreous haemorrhage.
Follow-up revealed additional, delayed effects of ocular trauma, including traumatic cataract and angle recession glaucoma.
Complications seen most frequently include:
Eyelid laceration:

Eyelid lacerations are defects in the eyelid that can be either partial or full thickness. They may also be accompanied by other ocular injuries such as corneal abrasions, disruptions of the surrounding structures, foreign bodies, penetrating eye injury, or orbital fractures.
Conjunctival and corneal injuries:
Ocular burn, corneal abrasions, and conjunctival and corneal foreign bodies are some examples of conjunctival and corneal injuries.
In contrast to minor wounds like abrasions and bruises that can heal with the help of lubricating drops and antibiotic drops, ocular burns and foreign bodies are more challenging to treat. It is important to treat eye burns as soon as possible. It might even require surgery if necessary.
The doctor has to inspect the eye for any type of foreign body, including those hidden in the eyelid’s deep grooves. An eye wash is often necessary to remove small particles that can cause allergies and infections in the eye.
Contusions and lacerations were the most frequent injuries to eyes, which included foreign bodies in the eye, according to a report.
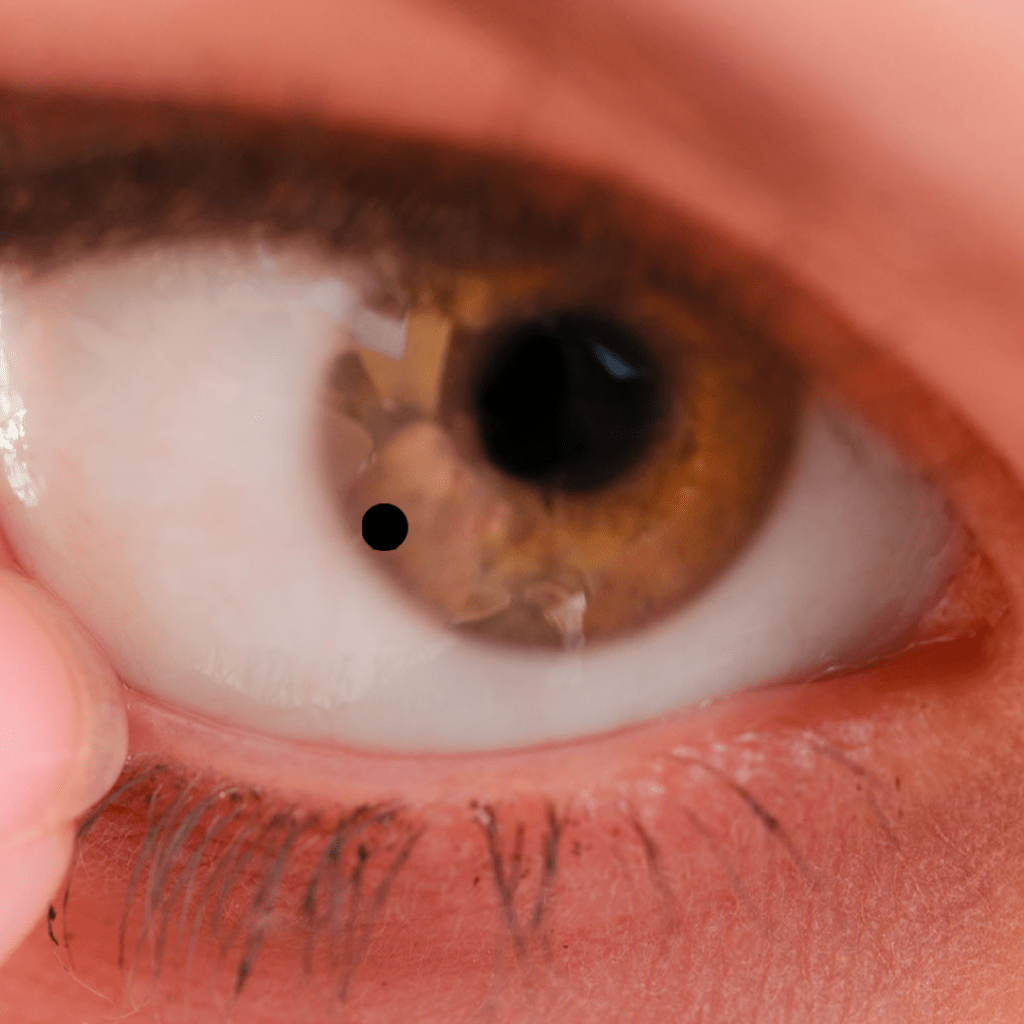
SUBCONJUNCTIVAL HAEMORRHAGE
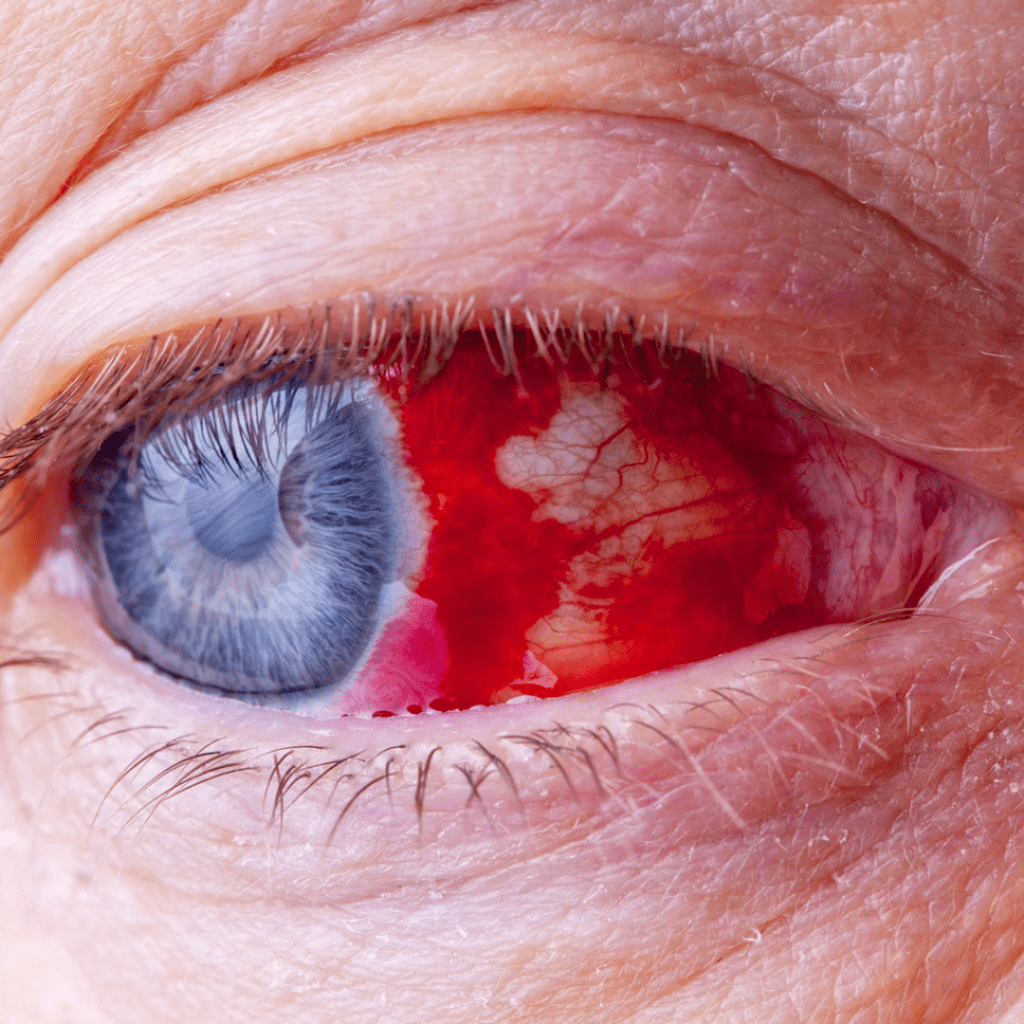
The conjunctiva’s blood vessels may burst as a result of trauma, which will result in blood accumulating there.
This causes the eyes to appear bloodshot. In a few weeks, this will naturally resolve.
Traumatic iritis:
The iris is a muscle in the eye that contracts and expands in response to certain stimuli such as light, causing the pupil to change size. In cases of trauma, this vascular iris becomes irritated, which triggers the production of inflammatory cells.
These inflammatory cells are also deposited on the cornea’s inner layer. Additionally, the inflammatory cells can obstruct the eye’s drainage angle, raising IOP and increasing the risk of secondary glaucoma in the affected person. A hypopyon, an anterior chamber filled with pus, can also form when precipitates accumulate in the anterior chamber.
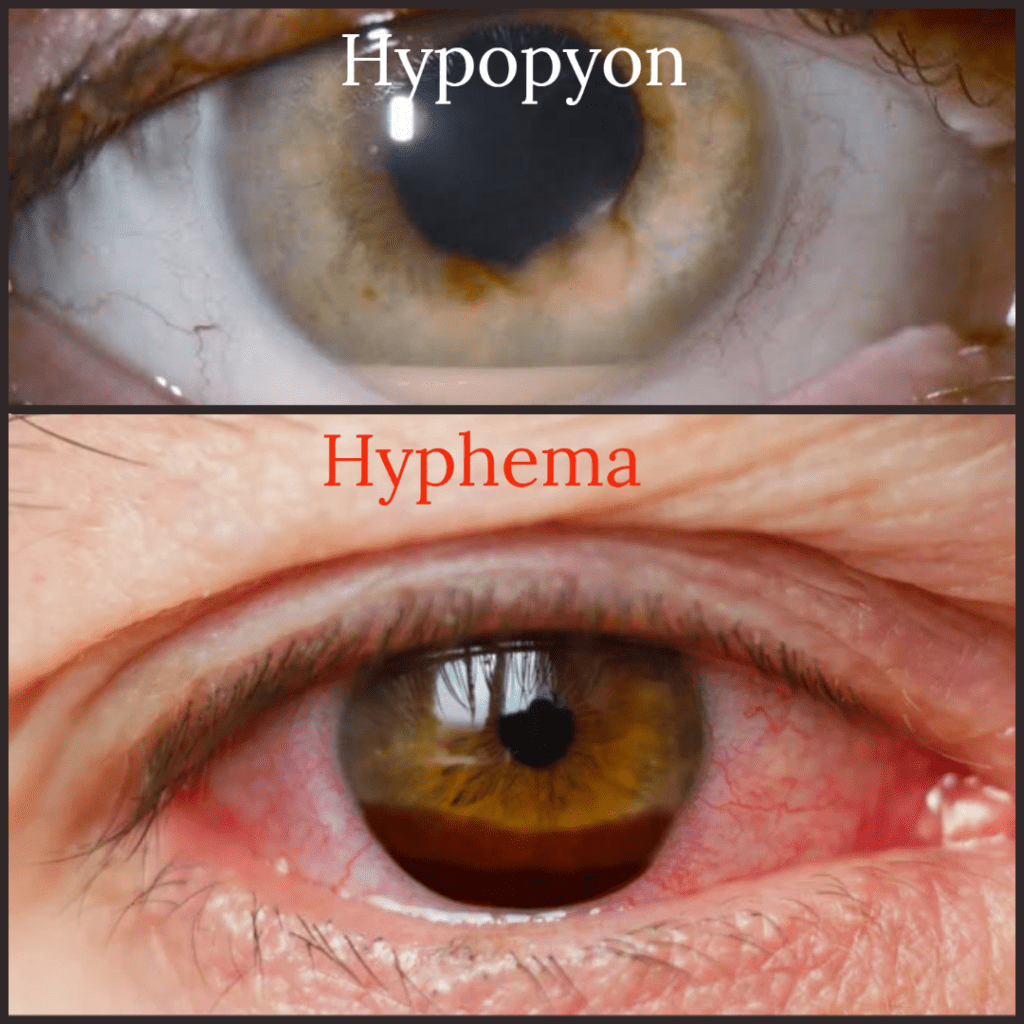
The treatment of traumatic iritis includes frequent use of steroidal eye drops, cycloplegics a few times a day, and IOP lowering drops.
Hyphema:
A hyphema is a buildup of blood in the eye’s anterior chamber. Blood can build up as a result of trauma to the ciliary body or iris blood vessels.
The hyphema is challenging to treat in people with sickle cell disease or other conditions that cause increased bleeding.
The height of the hyphema determines how it is graded. The likelihood of developing secondary glaucoma increases with the degree of hyphema because the red blood cells clog the draining angle.
The medical treatment of hyphema is similar to that of traumatic iritis, including topical steroids, cycloplegics, and IOP lowering drops.
In most cases, hyphema does not require surgery. Surgical removal of blood from the anterior chamber is imperative if uncontrolled glaucoma, corneal blood staining, hyphema persistence, or active anterior chamber bleeding are present.
Patients with sickle cell hemoglobinopathies and even those with sickle cell trait need surgery if intraocular pressure is not controlled within 24 hours.
Retrobulbar hematoma:
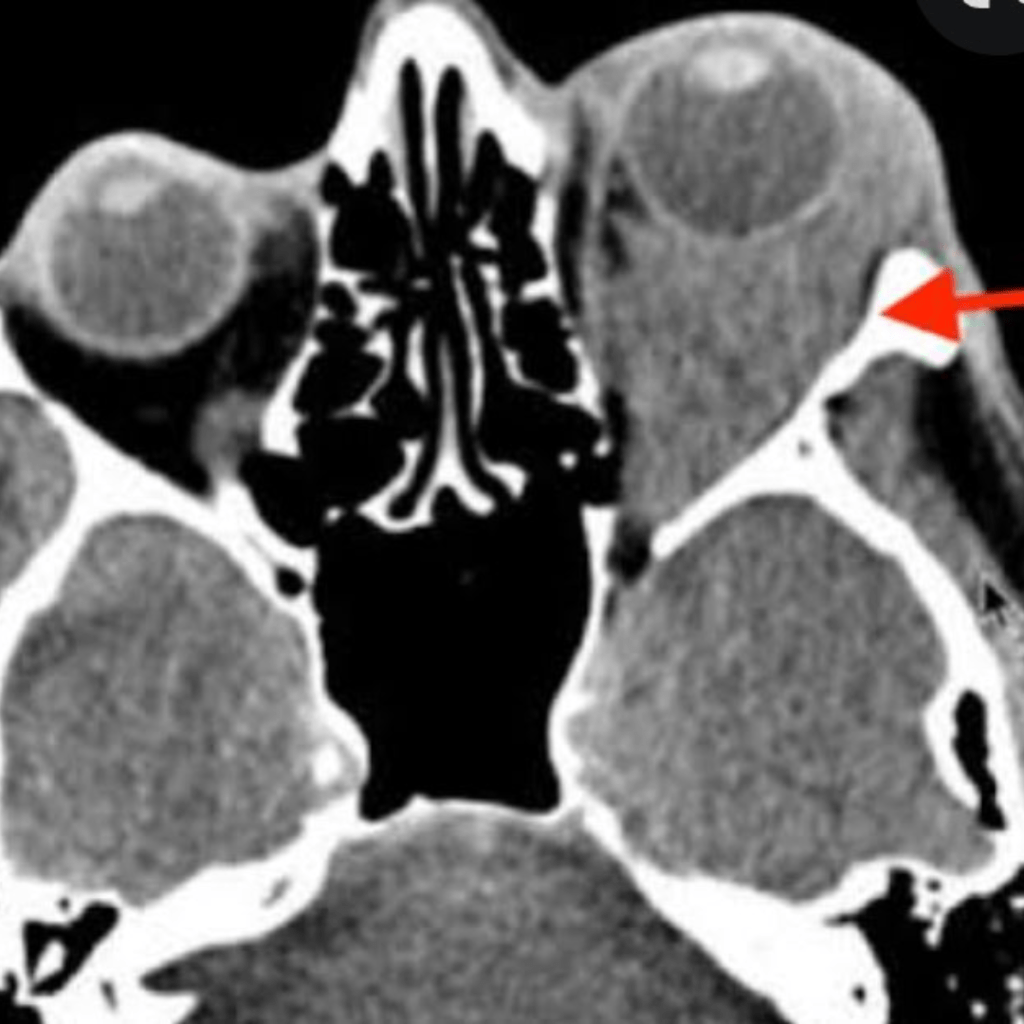
Firecracker injury may cause bleeding from the intraorbital artery, resulting in retrobulbar hematoma.
As a result of the blood accumulation posteriorly, the eye may end up protruding out. It could put the patient at risk for optic nerve compression, which could lead to vision loss.
A surgical procedure called lateral canthotomy that involves cutting the lateral angle of the eye, might be necessary to depressurize the orbit.
vitreous haemorrhage (VH):
This can occur as a result of blunt trauma or penetrating trauma.
Blunt trauma can cause bulging of the eye causing the vitreous to pull the retina inward, especially in young patients with formed vitreous and strong vitreous adhesion to the retina.
This inwardly directed tractional force applied to the retina by the vitreous can result in a split in the retinal layers or retinal dialysis, but it can also rupture retinal vessels and cause retinal tears and vitreous hemorrhage.
In case of penetrating injury a full-thickness eyewall defect brought on by blunt or sharp trauma can result in haemorrhage in all layers of the eye, including the vitreous.
Retinal detachment:
Like VH, there are two types of traumatic retinal detachments: those caused by a blunt contusion and those caused by a perforation of the eye’s posterior segment.
It is possible for retinal breaks to develop months or years after the trauma occurs. Performing repeated fundus examinations will help identify retinal breaks before retinal detachment occurs.
ANGLE RECESSION GLAUCOMA
Angle recession glaucoma (ARG) is caused by non-penetrating or contusive ocular trauma.
A receding anterior chamber, visible on gonioscopy, affects fluid drainage, which increases IOP. A small portion of those affected goes on to experience vision loss and glaucomatous optic neuropathy days, months, or even years later.
Compared to other types of glaucoma, angle recession glaucoma is typically harder to treat medically and surgically.
It is important to provide appropriate counseling and regular follow-up exams to patients who have suffered ocular trauma.
TIPS FOR PREVENTION
- Wearing protective eye goggles when bursting crackers.
- Always have an adult watch over kids using firecrackers. Keep young children, especially toddlers and the elderly away from firecrackers.
- Keep a safe distance when bursting crackers, don’t try to restart a firework that didn’t go off, wait at least a few minutes before approaching it.
- Never light a firework while holding it in your hands or pointing it at someone.
- Firecrackers should only be lit outside in an open area.
- Use only firecrackers purchased from authorized retailers and brands. Avoid purchasing unbranded firecrackers.
- Keep a fire extinguisher nearby at all times, or the very least, a bucket of water and sand to put out any stray flames.
- The fireworks should be ignited using long incense sticks instead of small match sticks.
- Do not touch or rub your eyes if you have been hurt. Instead, find a doctor right away and avoid attempting to treat any injuries yourself.
