NORMAL TEAR DYNAMICS:
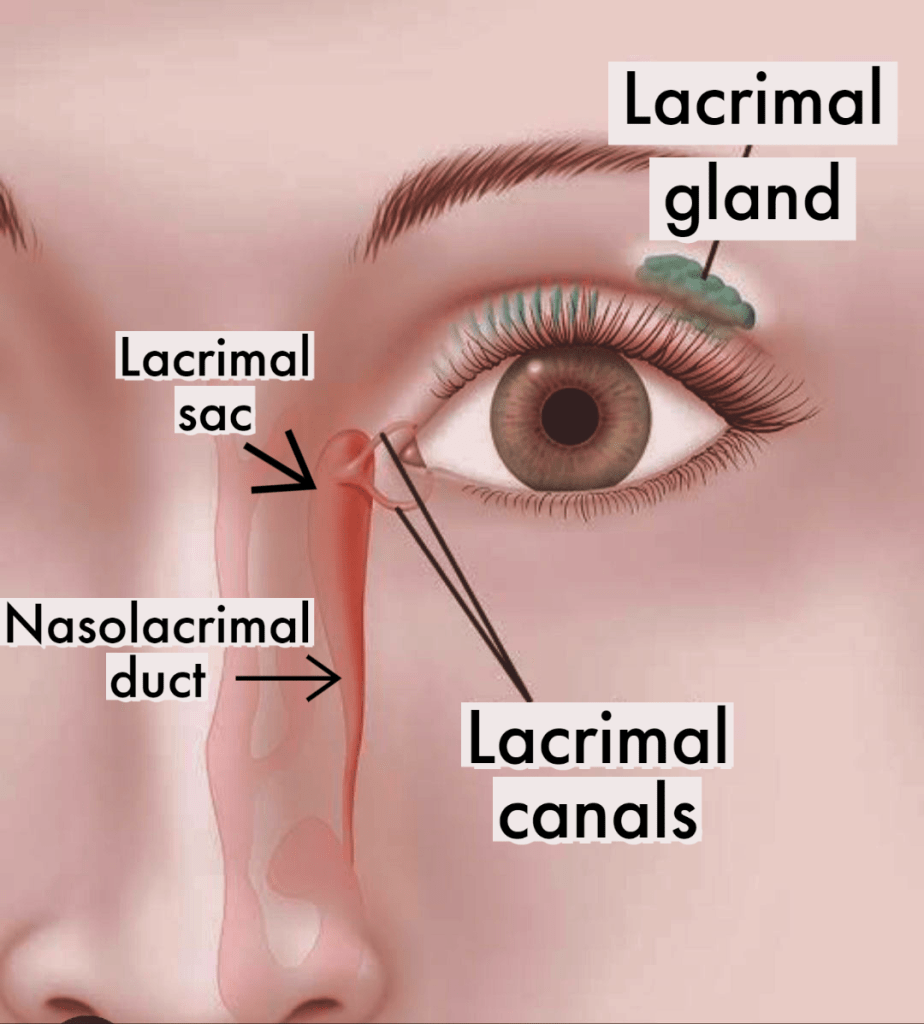
The lacrimal gland is responsible for making tears. Tears spread across the ocular surface as a result of the eyelids movement. The normal anatomy of the eyelid margins determines the proper tear passage.
The orbicularis oculi muscle controls eyelid closure. When the eyelid closes, the tear pump is activated.
As the eyelids close, tears in the margin of the eyelid are drawn into the lacrimal ducts through the punctum, and they are then pushed towards the lacrimal sac.
The sac contracts as the eyelids open, exerting the force required to push the tears into the nasal cavity via the nasolacrimal duct.
CAUSES OF WATERY EYES:
Epiphora is the medical term for excessive watering of the eyes. The cause is either inadequate tear drainage or excessive tear production.
Causes of insufficient tear drainage:
1. Eyelid misalignment:
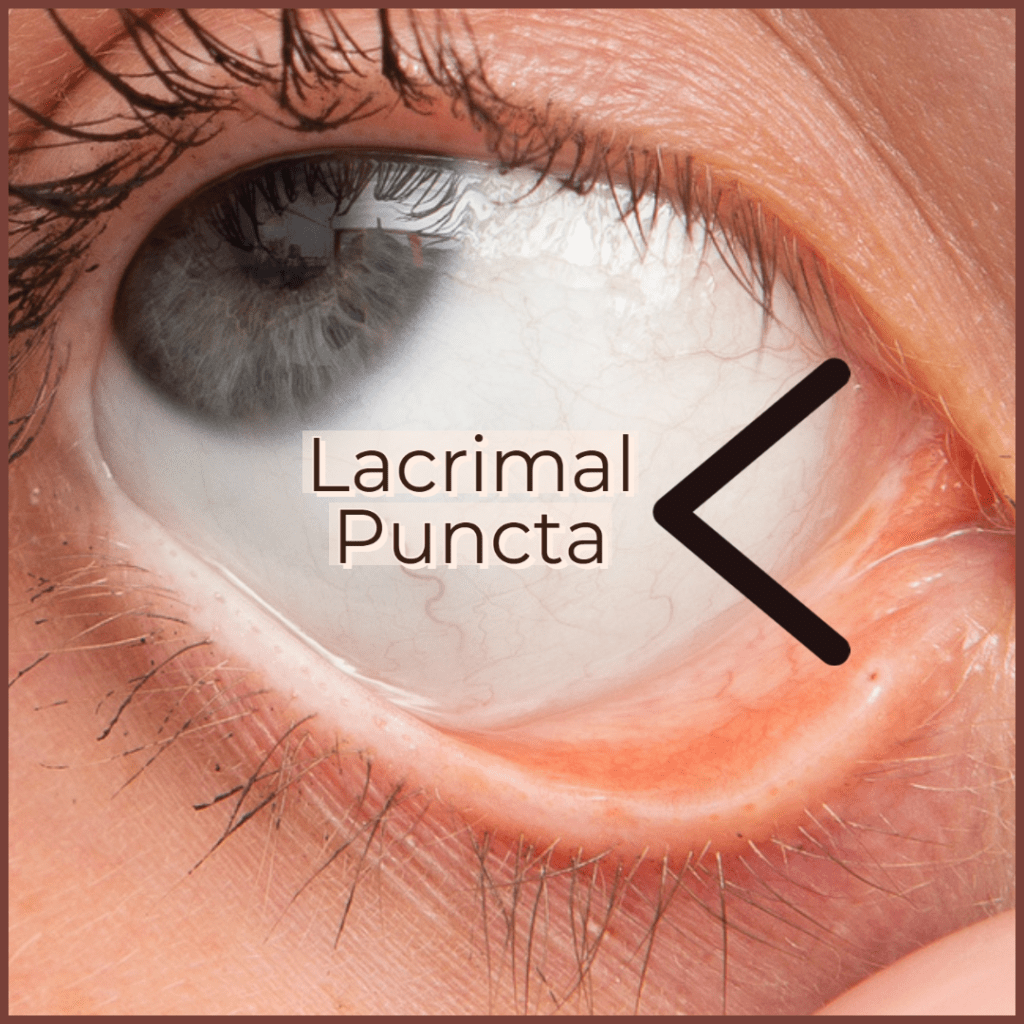
The lower lacrimal duct typically drains 90% of the tear fluid through the lower lacrimal punctum. Epiphora can be caused due to the misalignment of the eyelid margins or lacrimal puncta, even though the tear ducts are functioning normally.
Ectropion:
The condition of ectropion, or the outward turning of the lower lid, is common in older people due to loose skin and weakening of the eyelid muscles. This might also result from an infection, burn, or scar on the eyelids. The punctum turns outward, which causes the tears to fall as opposed to moving in the direction of the ducts.
Bell’s palsy:

Bell’s palsy is a condition that results in paresis of the facial nerve, or seventh nerve, which causes the muscles on one side of the face to suddenly weaken. This results in facial drooping and makes it difficult to make facial expressions like pouting or smiling. The orbicularis oculi muscle, which is supplied by the 7th nerve, is also affected. This impacts the tear dynamics and causes watering.
2. Lacrimal drainage system obstruction:
The tear drainage pathway includes the punctum, lacrimal ducts, lacrimal sac, and nasolacrimal ducts, which drain the tears from the lid into the nasal cavity.
Insufficient drainage and watering will result from an obstruction in any of these structures.
Nasolacrimal duct obstruction or NLDO is the most common cause of watering in infants. A baby’s tear duct may not be fully open and functional for the first few months of life, which will cause watering.
In adults, the same obstruction can be due to a tumor, mass, infection, or inflammation. An obstruction or restriction in the tear ducts prevents tears from draining properly and can cause tears to accumulate in the lacrimal sac.
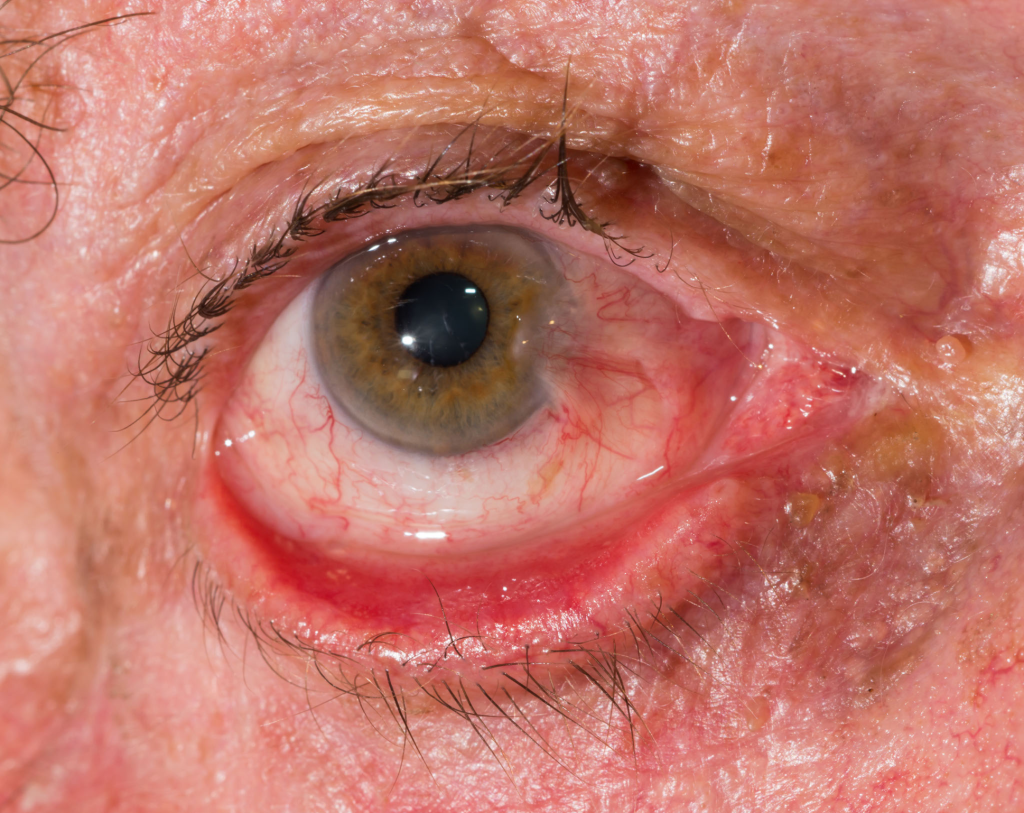
Stagnant tears in the tear sac increase the risk of infection known as dacryocystitis. This causes eye redness, eye discharge, lacrimal sac swelling, and pain, as well as the sensation of a foreign body in the eye.
Causes of excessive tear production:
The cause of excessive tear production is often crying, which is the result of an emotional state rather than a physical stimulus.
When the conjunctiva and cornea are stimulated, a reflex pathway opens, causing the lacrimal gland to release more tears. Common causes include:

- Eye allergies
- Dryness
- Eye infections
- Blepharitis
- Stye
- Inward turning of eyelashes or trichiasis
- Inward turning of lower eyelid or entropion
- Common cold
DIAGNOSIS:
1. Clinical diagnosis:
syringing:
After applying the local anesthetic eye drops, the doctor will pull down the lower eyelid to reveal the lower punctum.
The cannula which is connected to a saline-filled syringe, is inserted into the lower punctum. The patient will feel a salty liquid in their throat which they can swallow.
If the patient is unaware of this sensation, there is a blockage in the lacrimal apparatus somewhere.
2. Imaging method:
Dacryocystography (DCG), a common radiology procedure that uses contrast material, is the standard test for the diagnosis of lacrimal tract pathology.
Injecting contrast into the lacrimal system highlights the tear ducts and sac, allowing for the identification of the obstruction’s location.
TREATMENT:
Watery eyes might go away on their own. It is important to identify the cause of the increased production and begin the appropriate treatment.
This includes using artificial tears, warm compresses for dry eyes, antihistamines and cold compresses for allergies, antibiotic eye drops for infection, etc.
Correcting eyelid misalignment with surgery involves adjusting the muscles and tendons of the lid, resulting in the correct placement of the lid.
1. CRIGLER MASSAGE:

Crigler massage, a simple technique, can open up the NLDO in infants. By applying pressure to the nasolarimal duct, this massage can help the passageway open.
Remember to wash your hands first, and use a clean washcloth to clean the baby’s eyes.
Press the baby’s inner corner of the nose with your index finger and roll it down towards the nasal opening. Repeat five times on each side, three times per day.
2. PROBING:
Early probing is possible between the ages of 6 and 18 months.
When Crigler massage does not work after six to twelve months, the doctor may use the probing method.
During probing, the doctor may use a probe to open up tear ducts inside of one or both eyes that are either small or partially blocked. A total blockage of the ducts might require surgery.
Dacryocystorhinostomy (DCR) is the only treatment available for children with NLDO who don’t respond to massaging and repeated probing.
Most surgeons prefer to wait until the child is 3 years old before starting a DCR in order to avoid jeopardizing the bony growth.
3. DCR (dacryocystorhinostomy)

DCR surgery creates a new pathway between the tear sac and the nasal interior. As a result, tears bypass the blockage in the tear duct section.
The “gold standard” method of the procedure, external DCR (EXT DCR), involves creating a new opening after making an incision in the inside corner of the eye, connecting the lacrimal sac and nasal cavity, and then suturing the external incision.
Endoscopic DCR is another method of performing DCR. By inserting an endoscope into the nose, a new channel is created inside the nasal cavity from the lacrimal sac. Studies have demonstrated that endoscopic endonasal approaches are highly effective.
Stents can be implanted into this new pathway to keep the new channel open. The doctor can remove it later.
