According to the International Diabetes Federation (IDF), 1 in 10 adults worldwide suffer from diabetes and NIDDK (National Institute of Diabetes and Digestive and Kidney Diseases) has observed that about one in three diabetic patients older than 40 years have some changes in their retina related to high blood sugar.
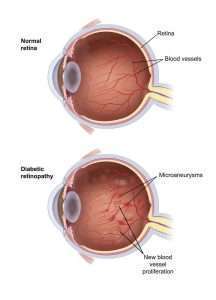
When diabetes affects the retina (the inner sensitive layer of the eye where light is perceived), it is known as diabetic retinopathy. This is a progressive condition and can lead to irreversible vision loss and even blindness.
What is diabetic retinopathy?
Diabetes and retina
Retinal arteries, which are blood vessels bringing blood to the retina, are damaged by the high glucose levels associated with diabetes. As a result, the arteries begin to leak, which causes hemorrhages and swelling (hard exudates, edema) inside the layers of the retina. The term for this is diabetic retinopathy.
What are the early signs of DR?
Many patients with DR might not even know that they have the disease. This is because it is usually symptomless in the early stages and can only be diagnosed with a dilated eye examination by an ophthalmologist.
In later stages, the patient can experience blurred vision and floaters.
Therefore, it becomes critical for a diabetic patient to get his/her eyes examined on an annual basis.
Once diagnosed with DR, further management depends on which stage the disease is at.
What are the types of Diabetic retinopathy?
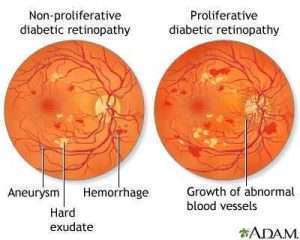
The DR is mainly of two types, non-proliferative and proliferative. The non-proliferative can further be divided into mild, moderate, and severe based on the findings.
NON PROLIFERATIVE:
The increased blood glucose in diabetes makes the retinal vessel wall weak resulting in an outpouching of the vessel lumen. These are seen as red dots in the retina and are called microaneurysms.
These microaneurysms may rupture and cause hemorrhages within the retinal layers.
The weak wall also starts leaking out proteins and lipids, which are seen as yellow deposits and swelling in the retina called hard exudates.
PROLIFERATIVE:
Increased retinal stress and the ensuing hypoxia or decreased oxygen level, result in non-proliferative to turn proliferative.
Vascular Endothelial Growth Factor (VEGF), a protein that plays a role in the development of new blood vessels, is produced in greater quantities in response to hypoxia to supply the retina with oxygen.
But these new vessels are fragile and therefore bleed easily, leading to even more devastating conditions like bleeding in the retina or the vitreous.
These new vessels in the retina can also pull it and cause retinal detachment.
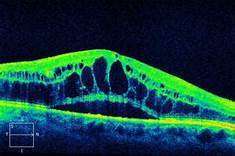
Diabetic Macular Edema (DME)
When the retinal vessels leak proteins and fats around the central part of the retina called the macula, which is responsible for the sharp central vision, it is known as DME.
This causes significant vision loss.
Symptoms of DR
Although DR is symptomless, there are some minor symptoms that you need to look out for, like
- Loss of vision
- Blurred vision
- Floaters or dark spots floating in front of the eyes
- Flashes of light
What are the tests required to diagnose DR?
The recommended guideline for the screening of DR in type 1 diabetic patients is an eye examination within 5 years of diagnosis and in type 2 diabetic patients, it is prompt screening right after diagnosis.
Generally, the longer you have diabetes, the more the chances are of having diabetic retinopathy. Therefore, even though the eye examination may be normal at a time, an annual eye check-up is critical.
The different tests used to diagnose DR are
- Dilated eye examination
- FFA
- OCT
Dilated eye examination:
After a slit lamp examination or direct eye examination through a microscope, your ophthalmologist will instill dilating drops in your eyes, which widens the pupils and helps the doctor to examine a large area of the back of your eyes, using an instrument called an indirect ophthalmoscope.
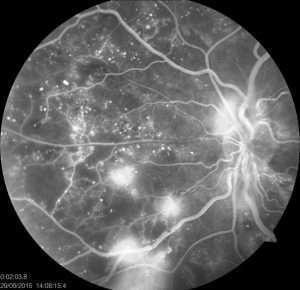
What is FFA?
FFA or Fundus Fluorescein Angiography is a technique in which dye is injected and photos of the retina or inner layer of the eye are taken at regular intervals. This is a very important diagnostic test to evaluate the type of diabetic retinopathy and its severity.
It can pick up new blood vessels at a very early stage, thereby enabling doctors to decide the best treatment option for their patients.
What is OCT?
Optical Coherence Tomography is a non-invasive imagining technique, which is important in measuring the swelling in the macula.
Post-treatment, this test is very useful for the doctor to assess how well the treatment has worked and if a repeat injection is required.
Treatment
In the mild-moderate type of nonproliferative diabetic retinopathy, a proper diet and prescription drugs (oral hypoglycemic/insulin) can be enough for treating diabetic retinopathy. A regular follow-up is inevitable.
In the severe type of diabetic retinopathy or PDR (proliferative diabetic retinopathy), along with good blood sugar control, laser treatment and/or anti-VEGF injection are required.
In DME with a focal leak, the leaky vessel is directly applied with a laser.
If DME is because of a diffuse leak, then anti-VEGF is injected.
What is anti-VEGF?
As mentioned earlier, VEGF is a molecule that causes the growth of fragile and leaky new vessels which can lead to hemorrhage and even detachment in the retina.
To avoid such devastating consequences anti-VEGF is injected into the eye which kills these molecules and helps halt the disease process.
These injections are given every month till the OCT shows complete regression of macular swelling.
Are anti-VEGF injections safe?
There are currently 3 widely available anti-VEGF
- Lucentis (ranibizumab)
- Avastin (bevacizumab)
- Eylea (aflibercept)
After various randomized trials (RESOLVE, RIDE, RISE, VISTA, VIVID, etc.), they are all considered to be highly efficacious and safe drugs.
How is anti-VEGF given?
1. Topical anesthetic drops are instilled. This makes the procedure painless. Only a little pressure is felt.
2. Topical antiseptic is instilled to make the eye surface sterile.
3. A sterile speculum is then applied that keeps the eyelids open.
4. A scleral marker is used to mark the site of entry on the white part of the eye or sclera.
5. A syringe with a very fine needle is used to deliver anti-VEGF in the eyes into the jelly or vitreous.
What is laser treatment?
Laser treatment is called PRP or Pan Retinal Photocoagulation. It is an outpatient laser procedure and is painless. It is usually carried out in 3 or more sessions.
The laser spots cause scarring in the peripheral retina which down-regulates VEGF. This even shrinks the fragile new blood vessels, therefore reducing the chances of complication and progression to the advanced stage.
What are the side effects of laser or PRP?
To avoid major complications, this procedure is carried out in sessions with 2-3 week intervals. Some known side effects of PRP are:
1. Decreased night vision
2. Reduction of visual field
3. Retinal detachment
4. Choroidal effusion
5. Macular edema
When is surgery indicated in DR?
Surgery is usually done in the advanced stages such as vitreous hemorrhage or tractional retinal detachment.
The surgery is called vitreoretinal surgery and is performed under local anesthesia.
What are the complications of DR?
If the disease continues, this can progress to the advanced stage. The complications include:
- Vitreous hemorrhage: The new fragile vessels can bleed into the jelly inside the eye, which is called a vitreous hemorrhage. One may notice many floaters in front of the eyes if the condition is mild or in severe cases, there can be loss of vision.
- Retinal detachment: The new vessels or scar tissue can even pull the retina and cause retinal detachment.
- Glaucoma: The VEGF can cause the growth of new blood vessels in the front part of your eye (iris) which may interfere with the drainage of the fluid out of the eye, causing increased pressure within the eye. This raised pressure can damage the nerve of the eye which is involved in image transmission to the brain. The condition is known as glaucoma
Can diabetic retinopathy cause blindness?
Yes, a complicated case of diabetic retinopathy along with diabetic macular edema/vitreous hemorrhage/retinal detachment/glaucoma or a combination of these conditions can lead to irreversible blindness.
What if one can’t afford anti-VEGF injection?
Yes, these injections are expensive and are required to be taken every 4-6 weeks till the swelling subsides. This can be a financial burden for many individuals.
In some cases, the doctor can suggest the combined treatment of anti-VEGF and PRP which is a better option, financially.
A quick summary:
Diabetic retinopathy and diabetic macular edema are debilitating eye conditions secondary to uncontrolled high blood sugar, leading to vision loss and even blindness. Good blood sugar control with proper diet and medication under physician guidance is very important.
There are two main types of diabetic retinopathy, non-proliferative and proliferative diabetic retinopathy. For severe non-proliferative diabetic retinopathy(DR), Proliferative Diabetic Retinopathy( PDR), and Diabetic Macular Edema(DME), the treatment modalities include laser(PRP) and anti-VEGF injections.
While surgery is reserved for the advanced stages such as PDR with vitreous hemorrhage or tractional retinal detachment, regular follow-up and treatment compliance by patients are inevitable to deliver the best visual outcomes.
If more help is required to understand this topic please feel free to reach out to us.
References:
1. https://www.ncbi.nlm.nih.gov/books/NBK560805/
2. https://pubmed.ncbi.nlm.nih.gov/29076303/#:~:text=
There%20is%20now%20strong%20evidence,VEGF%20drugs%20for%20proliferative%20DR.
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5712917/#:~:text=
In%20our%2015%20years’%20experience,allows%20a%20faster%20patient%20recovery
Disclaimer: The content on this site is for general information only and should not be used as a substitute for professional medical advice.