WHAT IS BLEPHARITIS?
Blepharitis is the inflammation of the eyelids. Symptoms may include eyelid redness, swelling, or a feeling of burning or soreness. In addition, affected individuals may have flakes or crusts at the base of their eyelashes.
TYPES OF BLEPHARITIS:
Lid margins have an anterior border, where the eyelashes are, and a posterior border, where meibomian glands open.
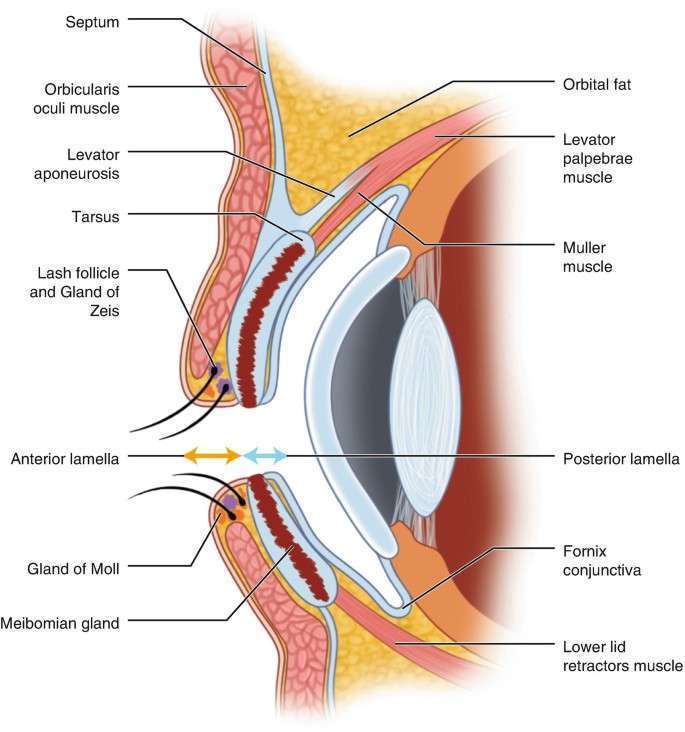
Each lid contains about 20-30 meibomian glands arranged vertically parallel to one another.
Sebum released by the meibomian glands forms a protective layer on the surface of the tear film that prevents it from evaporating fast.
Thus there are two types of blepharitis:
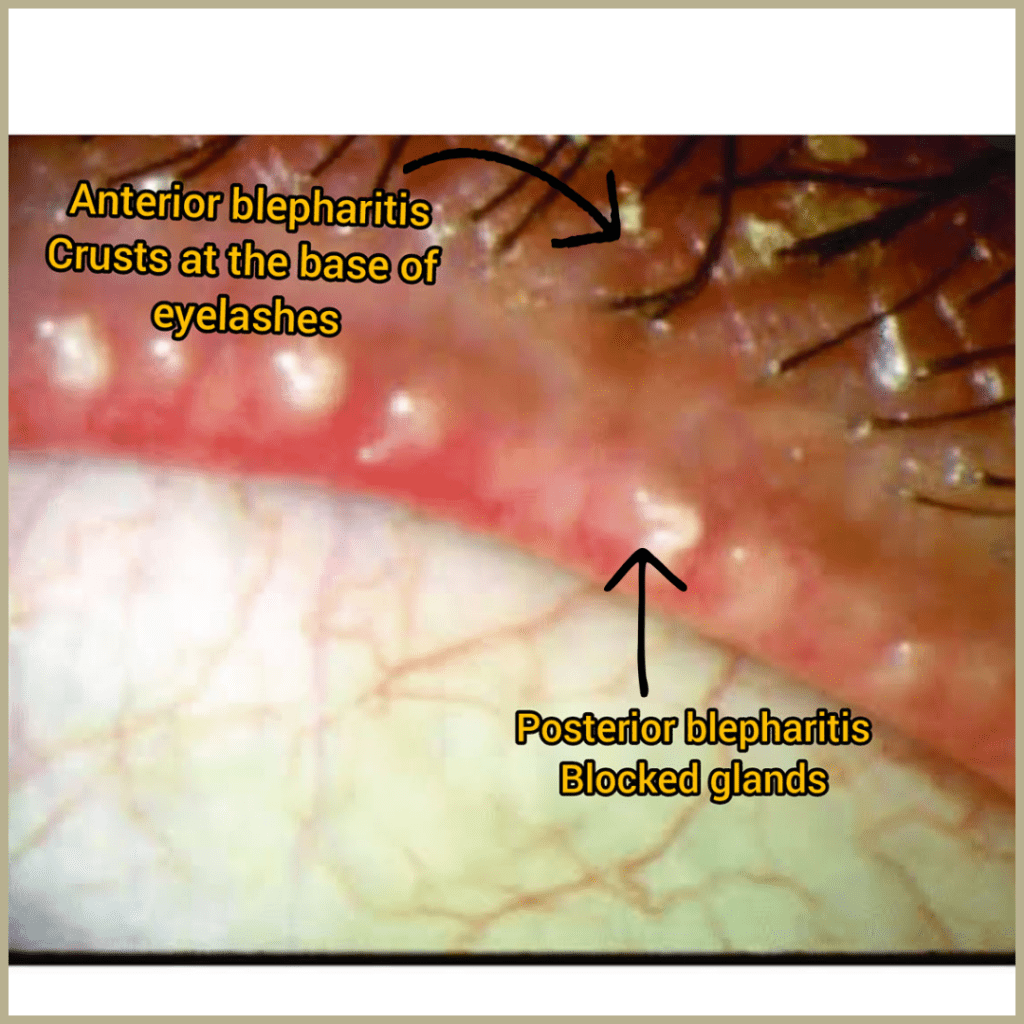
Anterior Blepharitis: Involving the anterior border of eyelids and eyelashes
Posterior Blepharitis: Inflammation of meibomian gland or meibomitis
symptoms:
1. Dry eyes:
Whenever we blink, our meibomian glands squeeze out the oily secretions or sebum that help maintain the tear film’s stability.
Due to blocked glands, the tear film becomes unstable, evaporates faster causing dry eye.
2. Tearing:
Oil from these glands also thickens tears, preventing them from overflowing across the lid margin. As a result of blocked glands, tears will be thinner in consistency and may overflow from the lid margin.
3. Crusting:
Oil bacteria and dead cells cause crusts to form. It can cause irritation, watering, burning, and discomfort, redness of the conjunctiva and inflammation of the eyelid margin.

4. Blurred vision:
Rarely, the cornea becomes irritated with inflammation and infiltrates causing light sensitivity and blurred vision.
5. Compromised lashes:
The crusts and dandruffs cause loss of lashes and misdirected lash growth
SIGNS
Anterior blepharitis: Crusty, red thickened eyelid margins
Posterior blepharitis: Anterior blepharitis is frequently present along with prominent blood vessels and thickened oil glands on the posterior eyelid margins.

Mites in eyelids: Demodex mites can cause anterior (Demodex folliculorum) and posterior (Demodex brevis) blepharitis
Less common signs:
- Redness in conjunctiva
- Swelling in eyelids
- Mild mucous discharge
- Superficial punctate keratitis
- Rosacea
- Corneal infiltrates
ETIOLOGY:
Blepharitis occurs in people of all ages and ethnicities, but women in the 40-50 age group are more likely to develop it. Also, Individuals with ocular allergies, oily skin, rosacea, or dandruff are more likely to develop blepharitis.
Anterior blepharitis are of following types depending upon the etiology
- Staphylococcal bacterial infection: Common sign is crusting along the eyelashes
- Seborrheic disease: individuals have seborrheic dermatitis of the face and scalp.
- Associated with rosacea.
Posterior blepharitis:
Meibomian gland dysfunction causes posterior blepharitis. Thickened secretions clog and engorge the glands. Often, acne rosacea is associated with this, and hormonal causes are suspected.
DIAGNOSIS
Usually for diagnosing blepharitis a physical exam and history are sufficient.
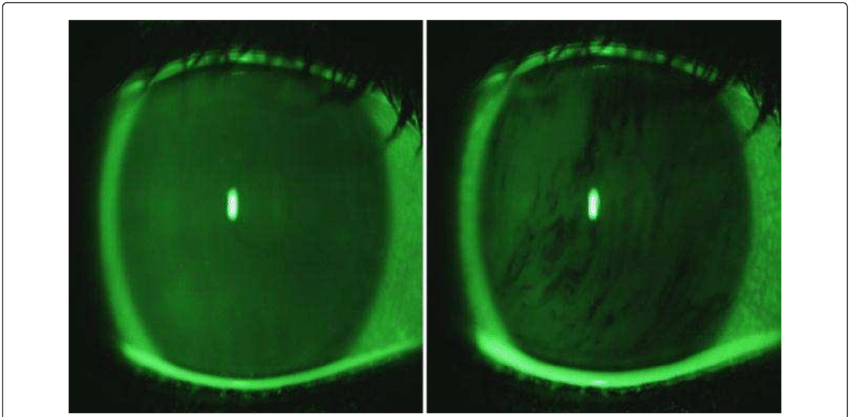
Blepharitis causes the tear film to evaporate rapidly. The best way to assess this is by measuring the tear break-up time or TBUT.
A slit-lamp examination is done after fluorescein dye is added to the patient’s eyes. After blinking fully, the patient must avoid blinking for 10 seconds. Under cobalt blue filter, the tear film is examined for any breaks or dry spots. Tear break-up time less than 10 seconds are generally considered abnormal.
MANAGEMENT:
Blepharitis is not a serious health threat. It can be managed at home and requires everyday self care.
Self care/ Home remedy includes:
- Warm compresses/heated eye mask for 5-10 minutes 2-4 times a day for 2 weeks
- Lid scrubs: Use lid wipes or hypochlorous lid spray and wipe with a clean washcloth along the lid margin. Massaging the lid margins is very important.
- When dealing with demodex mite infestations, use tea-tree oil lid scrubs or hypochlorous acid eyelid cleaning solutions once or twice each day for six weeks.
- Lubricating eye drops for burning and discomfort
- If you wear eye makeup, make sure to clean your lid margin before going to bed.
- Contact lens wearers must wash their hands with soap and water before wearing the lenses.
Medical care:
1. Blepharitis with moderate severity may require azithromycin or erythromycin eye ointment.
2. Vitamin supplements such as omega 3 fatty acids are anti-inflammatory and can help treat blepharitis.
3. Treatment for severe or non-responding blepharitis includes an oral antibiotic such as doxycycline (not recommended for pregnant or nursing women and children <8 years) or azithromycin/erythromycin coupled with steroid and antibiotic eye ointment.
4. If there is little or no improvement with abovementioned treatment then management includes thermotherapy to the meibomian gland with expression, laser therapy, microblepharoexfoliation, and meibomian gland probing.
CARCINOMA OF THE EYELID

If chronic blepharitis fails to respond to treatment, a biopsy of the lid should be done to exclude carcinoma, especially in cases of loss of eyelashes.
As sebaceous carcinomas of the eyelids rarely manifest as intractable, unilateral, or asymmetric blepharitis, it’s vital to get your eyes checked by a registered eye practitioner.
