Diabetes is one of the major causes of blindness, kidney failure, heart attacks, strokes, and lower limb amputations. Uncontrolled diabetes frequently causes hyperglycemia or raised blood sugar, which over time can seriously harm many different bodily systems, particularly the nerves and blood vessels.
Uncontrolled blood sugar leads to the following conditions in the eye:
1. SUBCONJUNCTIVAL HAEMORRHAGE:
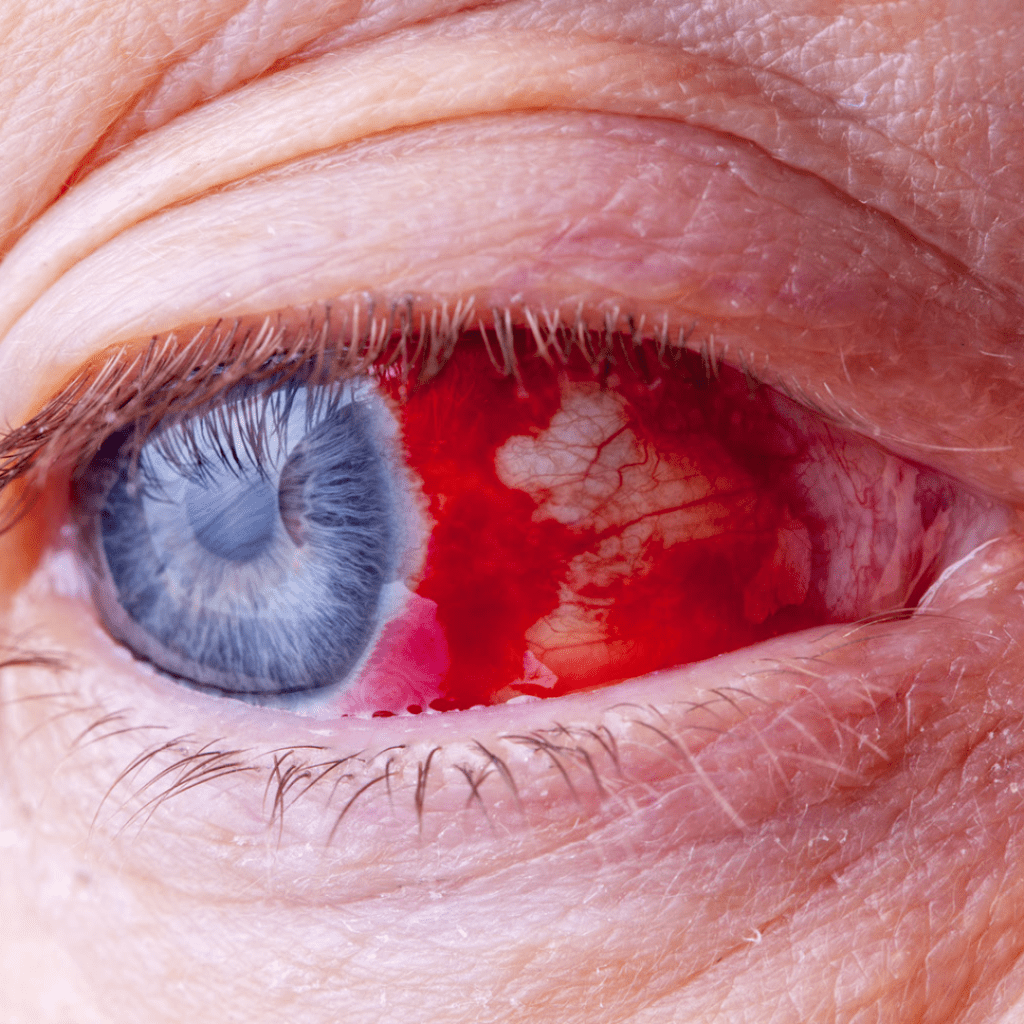
Conjunctiva is the translucent, lax membrane covering the white part of the eye. Under the conjunctiva, minute blood vessels are visible to the naked eye.
For some reason, when these blood vessels rupture, there is an accumulation of blood under the conjunctiva. As a result, the eye appears bloodshot.
The main causes of spontaneous SCH are hypertension and other vascular diseases like diabetes and hyperlipidemia. These illnesses may weaken and spontaneously burst blood vessels.
Despite the fact that it might seem risky, this usually isn’t cause for concern and goes away in a few weeks.
2. DIABETIC RETINOPATHY:
The retinal arteries carry blood to the retina. Due to increased blood glucose, the walls of these arteries weaken. As a result, the vessels begin to leak, which causes hemorrhages and swelling (hard exudates, edoema) within the layers of the retina. The term for this is diabetic retinopathy.
Non-proliferative and proliferative DR are the two main types.
- Non Proliferative diabetic retinopathy (NPDR):
Diabetes causes the retinal vessel wall to become weak, which causes the vessel lumen to protrude outward, a condition known as microaneurysms. Retinal microaneurysms appear as red dots.
When these microaneurysms burst there are retinal hemorrhage within the retinal layers.
Proteins and lipids leak from the weak retina wall, causing yellow deposits known as hard exudates.
- Proliferative Diabetic retinopathy (PDR):
Now that the retina is under so much stress, there is a deficiency in oxygen, which causes the release of VEGF (Vascular Endothelial Growth Factor), which has the function of creating new blood vessels.
These new vessels, however, are weak and prone to bleeding, which can result in even more serious conditions like bleeding in the retina or vitreous.These new vessels in the retina can also pull it and cause retinal detachment.
In the mild-moderate type of non-proliferative diabetic retinopathy, a proper diet and prescription drugs (oral hypoglycemic/insulin) can be enough for treating diabetic retinopathy. A regular follow-up is inevitable.
The most severe types of diabetic retinopathy, such as PDR (proliferative diabetic retinopathy), require laser surgery and/or anti-VEGF injections in addition to good blood sugar control.
3. DIABETIC MACULAR EDEMA (DME)
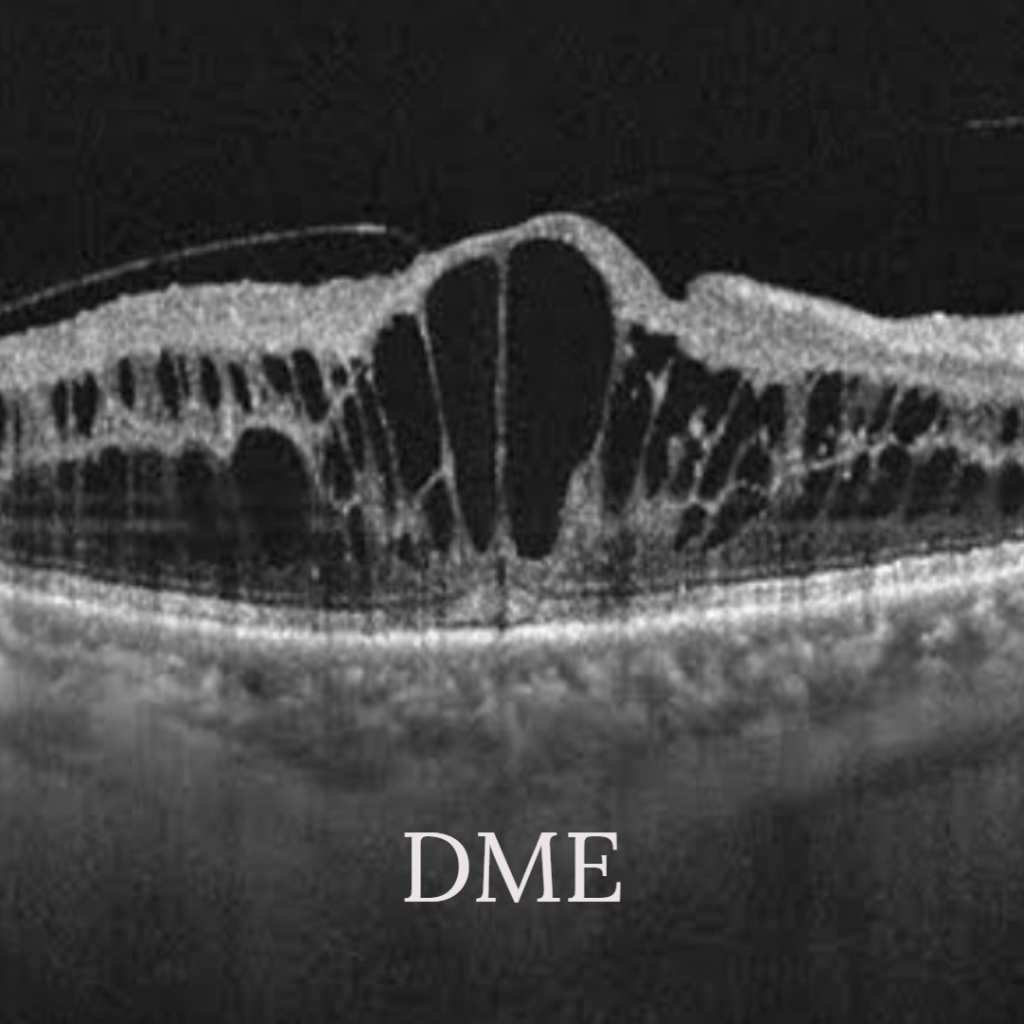
DME is a condition where the retinal vessels around the macula, the center of the retina and the source of sharp central vision, leak proteins and fats. Significant vision loss results from this.
Optical Coherence Tomography is a non-invasive imagining technique, which is important in measuring the swelling in the macula.
For focal leaks, lasers are used directly to close the leaky vessel, but for diffuse leaks, anti-VEGFs offer better treatment options.
4. Recurrent Stye:

A hordeolum, also known as stye, is swelling of the lids caused by an infection, while a chalazion is inflammation of the eyelids that is not infectious.
Patients who suffer from long-term illnesses like diabetes, seborrheic dermatitis, and high serum lipid levels could also be at higher risk.
The person should get blood tests because recurrent stye can sometimes be the first sign of diabetes.
Small swellings inside the eyelids are a symptom of another condition known as a chalazion. This condition is not painful, unlike a stye, but if diabetes is persistently high levels, it may become painful and infected.
5. CATARACT:
The most common cause of blindness and one of the main factors contributing to visual impairment in diabetic patients is the cataract. According to reports, patients with DM have a five times greater chance of developing cataracts, especially when they are young.
What causes cataract in diabetic patients?
The lens must be clear and transparent for the light to focus on the retina. Sorbitol is produced in the lens from glucose. Due to its high osmotic nature, sorbitol must be broken down through metabolism.
The enzyme sorbitol reductase is responsible for this metabolism to fructose.
Due to the high glucose levels in diabetic patients, sorbitol production is increased. A hyperosmotic effect caused by the increased intracellular sorbitol accumulation causes more fluid flowing into the lens, causing opacity.
Additionally, elevated glucose concentrations in the aqueous humor may cause lens proteins to glycate, which generates advanced glycation end products.
6. POST CATARACT SURGERY COMPLICATIONS:
- Cystoid macular edema (CME):
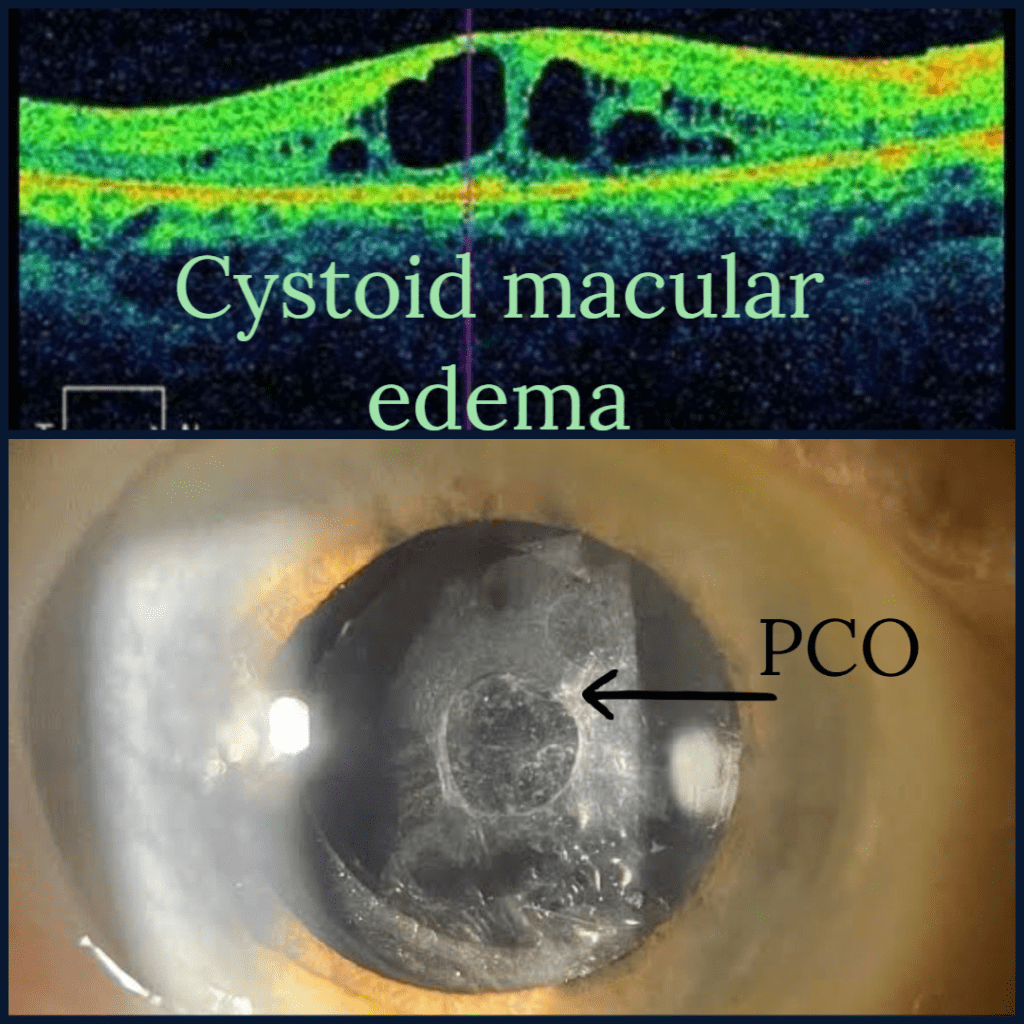
It is common to observe postoperative macular edema (CME) following cataract surgery. However, compared to the general population, patients with diabetes experience a more extended recovery period, a need for medication, and close monitoring of their condition.
In addition to having a higher risk of developing CME, diabetic patients with DME are more likely to experience worsening edoema after cataract surgery.
- PCO (Posterior capsular opacification):
The most frequent complication following cataract extraction is posterior capsule opacification (PCO), also known as “secondary cataract.”
Following cataract removal, the remaining lens cells migrate, proliferate, and differentiate behind the artificial lens on the posterior lens capsule, resulting in PCO.
According to some studies, PCO is more likely to develop in diabetic patients and become more severe than in non-diabetic patients.
This is most commonly treated with a laser procedure.
- Decompensation of the cornea:
After cataract surgery, corneal endothelial cell damage and persistent corneal edema have become more common in diabetic patients. Therefore, specular microscopy should be used to evaluate DM patients, and all intraoperative precautions should be taken.
- Increased inflammation:
Severe iritis, posterior synechiae, pupillary block, and pigmented precipitates on the IOL are also more frequently seen in diabetic patients.
7. Recurrent corneal erosions:
Patients with dry eye syndrome, diabetes mellitus, blepharitis, and ocular rosacea have the highest rates of recurrent corneal erosion (RCE).
Reduced corneal sensitivity has been linked to diabetes mellitus types 1 and 2. Due to impaired corneal sensation, corneal epithelial defects and persistent erosions are more common as the patient’s age and diabetes duration rise.
Despite having corneal pathology or epithelial defects, these patients typically report little to no ocular discomfort.
Aggressive lubrication, as well as antibiotic and blood serum drops, are all part of the treatment.
8. CRANIAL NERVE PALSY
In diabetic patients, ophthalmoplegia is a form of microvascular cranial nerve palsy (cranial nerve III, IV, and VI) causing weaking of eye muscles and restricted eye movements. However, full recovery usually occurs within 12 weeks of the onset of symptoms.

According to numerous reports, cases of ophthalmoplegia were significantly more likely to have either mild (NPDR) or sight-threatening (PDR and ME) diabetic retinopathy. The fact that both diseases result from the microvascular abnormalities linked to diabetes and its related co-morbid factors may help to explain why retinopathy occurs frequently in cranial palsy cases.
The following were the risk factors for developing cranial nerve palsies in this study:
Risk factors:
- Age >45 years
- Diabetes duration ≥ 10 years
- male gender
- DR
- Diabetic nephropathy
- Less significant risk factors include obesity and poor glycemic control
- Hypertension is not a risk factor but may worsen the effect of diabetes in ischemic nerve palsies
This study shed more light on the prevalence of ophthalmoplegia, its various cranial nerve palsies, and the crucial risk factors that clinicians should take into account when performing screening tests for this uncommon condition.
9. PRIMARY OPEN ANGLE GLAUCOMA (POAG):
The blue mountains eye study Australia suggests that there is a true connection between Diabetes and POAG through unknown mechanisms.

Several theories have been proposed regarding the biological connection between glaucoma and diabetes.
The suggested theories are as follows:
- Microangiopathies result from diabetes. Due to the reduced blood flow to the retina and optic nerve, the retinal cells (also known as retinal ganglion cells, or RGC), which transmit visual information to the optic nerve, receive less oxygen and nutrients. This would lead to RGC degeneration and the start of glaucomatous impairment.
- Second, there is a tonne of evidence that diabetes-related hyperglycemia and lipid abnormalities can increase the risk of neuronal injury, suggesting that diabetic patients have a higher risk of RGC death.
- Third, the increased glucose in the aqueous humor in diabetic patients’ eyes would promote the production and accumulation of fibronectin to encourage the loss of trabecular meshwork cells, which might impede the aqueous humor’s outflow system and ultimately lead to POAG.
QUICK SUMMARY:
Diabetes can result in severe eye conditions as a result of unchecked blood sugar levels, which can cause vision loss and even blindness. Under the direction of a doctor, maintaining good blood sugar control with a healthy diet and medications is crucial.
