People who prefer not to wear glasses can greatly benefit from contact lenses especially those with high refractive errors. Contact lenses are a great alternative for those who want good eyesight without compromising their range of vision. It’s important to be aware of the risk of eye infections from incorrect contact lens use. Good hygiene, regular washing, and disinfection of contact lenses are crucial for maintaining good vision.
The following is a list of 9 issues related to contact lens use.
1. Corneal Infections and ulcer
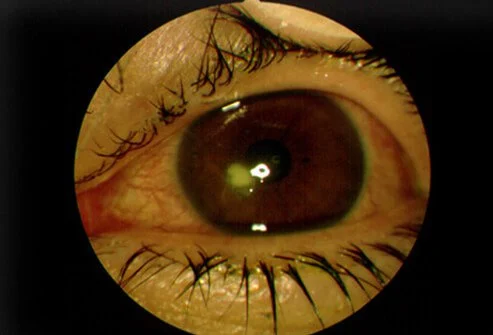
Microbial Keratitis (MK) is an uncommon but significant contact lens problem that can cause corneal scarring and lead to vision loss.
Contact Lens Peripheral Ulcer (CLPU) is a less dangerous but more frequent complication. MK and CLPU are both caused by an inflammatory response in the cornea.
The symptoms, which are milder in CLPU and more severe in ML, include redness, discomfort, watering, irritation, and foreign body sensation.
When the lesion is cultured, the MK shows growth of microorganisms while CLPU is mostly culture negative, indicating that CLPU is a sterile ulcer. Although Staphylococcus aureus and the CLPU have occasionally been linked.
While MK requires more aggressive care with antibiotics and non steroidal or steroidal medications and close follow-up, CLPU is self-limiting and resolves on its own after discontinuing contact lens usage.
2. Hypoxia
The cornea receives its oxygen from the atmosphere, therefore having contact lenses that are overused, tight or made of poor material results in hypoxia or low oxygen environment in cornea.
The layers of the cornea get clogged with fluid due to hypoxia which results in corneal clouding and possibly scarring.
3. Corneal neovascularzation

Neovascularization of the cornea refers to the development of new blood vessels around it. This happens as a result of hypoxia, and the body attempts to provide the cornea with additional oxygen by creating new vessels. But because these vessels are abnormal, wearing contact lenses must be stopped until they recede.
4. GPC (Giant Papillary Conjunctivitis):
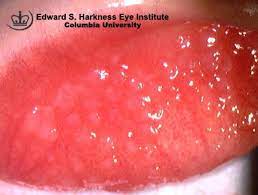
Contact lenses can cause mechanical damage to the superior tarsal conjunctiva as well as hypersensitivity reactions to allergens or proteins deposited on the lens surface.
Overuse of contact lenses, wearing them while sleeping, poor cleanliness, tears’ proteins adhering to the contact lens surface, and biofilm formation are some of the causes.
The papillae in the conjunctiva of the upper eyelid are larger than those seen in allergic or bacterial conjunctivitis. They resemble cobblestones in appearance.
Symptoms include itchiness, discharge, redness, fluctuating eyesight, mucus discharge upon waking, a feeling of a foreign body, and redness.
Treatment options include avoiding contact lenses for few weeks, and applying a topical steroid, mast cell stabilizer, or antihistamine and switching to daily disposable rather than extended wear contact lenses.
5. Contact lens-associated red eye
Red eye from wearing contacts is generally felt shortly after waking up from sleep. Mild discomfort, burning, and photophobia are some of the symptoms.
Long-term use, inadequate lens cleaning, germs attached to the lens releasing toxins, and buildup of byproducts while the eyes are closed while sleeping are some of the causes.
Management includes stopping the contact lenses and using lubricants for soothing the eyes. the prognosis is good and recovery will take 1-2 weeks.
6. Corneal warpage
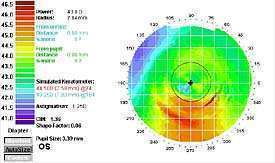
The look of the corneal topography maps can be used to detect corneal warpage since they often display bilateral, somewhat symmetrical superior flattening and striking inferior steepening.
A thorough history, examination, and follow-up are crucial since the corneal warpage on topography exhibits maps that are strikingly similar to keratoconus. Therefore identifying corneal warpage on topography due to contact lens wear before switching to alternative methods of correcting refractive error, such as soft toric, multifocal contacts, orthokeratology, or refractive surgery is important for proper management.
7. Allergic conjunctivitis:
Thimerosal, a preservative found in various lens cleaning solutions, is a common allergen that causes allergic conjunctivitis. The patients would have foreign body sensation, Papillar conjunctivitis, redness, watering, itching, and burning.
Alternative contact lens cleaning solutions, topical antihistamines, topical steroids, temporary contact lens discontinuation, or moving to daily disposable lenses are all examples of management options.
8. Displaced contact lens:

Displaced contact lenses can migrate, decenter, and even move into the superior fornix. Therefore it is crucial to have a consultation on proper fitting by a registered eye practitioner before regularly using a contact lens.
A poorly fitting contact lens might have harmful repercussions. For instance, a decentered contact lens can cause mechanical damage to the cornea, compromising its surface and making it vulnerable to infections and inflammatory reactions
9. ptosis:
Ptosis is drooping of upper eyelid and aponeurotic is problem of eyelid muscle called Levator palpebral superioris or LPS aponeurosis.
It is well accepted that using contacts for a prolonged period of time can cause acquired ptosis. Although a few of these incidents have been connected to soft contact lenses, hard lenses are the more frequent offender.
Contact lens-induced ptosis can be diagnosed in contact lens wearers who present with acquired ptosis without a history of ocular surgery, illness, muscle and neurological problems, or trauma.
RISK FACTORS OF CONTACT LENS RELATED COMPLICATIONS:
- Bad CL fitting (tight or loose)
- Co- existing active corneal pathologies (infections, abrasions)
- Allergies
- Solution preservatives
- In contact lens that is misused excessively or is not cleaned thoroughly, proteins, bacteria, and inflammatory mediators from tears form a biofilm on the lens surface.
- Overusing and abusing of CL
- Sleeping with CL
- Swimming with contact lenses
MANAGEMENT
- Proper cleaning and sterilizing of contact lens. Read 7 PROS AND CONS OF GLASSES AND CONTACT LENSES
- Avoid wearing contact lenses till the eyes heal
- Switch to daily wear from extended wear
- Lubricating drops for relief
- Topical antimicrobials in keratitis
- Non steroidal anti-inflammatory or steroidal medications
- Antihistamines or mast cell stabilizers in case of allergies
- Use of glasses two days prior to getting corneal topography
QUICK SUMMARY:
While using contact lenses allows you a great deal of flexibility, there are numerous considerations to make in order to get the most out of them. This includes taking them off before going to bed and wearing them for no more than 12 hours every day. Storing them in a disinfected container and handling them with clean hands. Adequate cleaning and disposal practices are necessary in order to use contact lenses to their maximum capacity.

